 Journal of Medical Research and Surgery
PROVIDES A UNIQUE PLATFORM TO PUBLISH ORIGINAL RESEARCH AND REMODEL THE KNOWLEDGE IN THE AREA OF MEDICAL AND SURGERY
Journal of Medical Research and Surgery
PROVIDES A UNIQUE PLATFORM TO PUBLISH ORIGINAL RESEARCH AND REMODEL THE KNOWLEDGE IN THE AREA OF MEDICAL AND SURGERY
 Journal of Medical Research and Surgery
PROVIDES A UNIQUE PLATFORM TO PUBLISH ORIGINAL RESEARCH AND REMODEL THE KNOWLEDGE IN THE AREA OF MEDICAL AND SURGERY
Journal of Medical Research and Surgery
PROVIDES A UNIQUE PLATFORM TO PUBLISH ORIGINAL RESEARCH AND REMODEL THE KNOWLEDGE IN THE AREA OF MEDICAL AND SURGERY
 Indexed Articles
Indexed ArticlesSelect your language of interest to view the total content in your interested language
Sebastián Rosero Cabrera1*, William Pinzón Gallardo2, Helberth Augusto González Rico3, Carlos Fernando Bastidas Gómez4, Tulio Sotomayor Medina5, Andrea Carolina Wilcox Robles6, Decknia Luz Vásquez Moris6, Carlos José González Tejeda7
1General Physician, Universidad de Antioquia, Colombia
2General Physician, Universidad Surcolombiana, Neiva-Colombia
3Resident Physician of Orthopedics and Traumatology, Universidad del Rosario, Bogotá, Colombia
4General Physician, Universidad Cooperativa de Colombia, Colombia
5General Physician, Universidad Metropolitana de Barranquilla, Colombia
6General Physician, Universidad Libre de Barranquilla, Colombia
7General Physician, Fundación Universitaria San Martín
Correspondence to: Sebastián Rosero Cabrera, General Physician, Universidad de Antioquia, Colombia.
Received date: November 05, 2021; Accepted date: November 19, 2021; Published date: November 26, 2021
Citation: Cabrera SR, Gallardo WP, Rico HAG, et al. (2021) Use of External Approach for Severe Genu Valgo Knee Arthroplasty. J Med Res Surg 2(6): pp. 1-4. doi: 10.52916/jmrs214061
Copyright: ©2021 Cabrera SR, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License; which permits unrestricted use; distribution and reproduction in any medium; provided the original author and source are credited.
The deformities of the lower limbs (genu valgus and genu varus) are alterations frequently developed properly by physiological processes which usually disappear at 2 years (genu varus) and at 7-8 years (genu valgus), being considered in adults normal a 4º-6º genu valgus, however the appearance of the latter is also related to various metabolic pathologies, tumors, traumatic sequelae, infections, skeletal dysplastic and idiopathic genu valgus. In the bibliography, there is a greater consensus on the approach to varus deformity, not so in valgus deformities, where there is no bibliography with a level of evidence that defines established protocols to treat severe valgus deformities>20, currently good treatment results have been demonstrated by means of knee arthroplasty to correct genu valgus deformities, which showed good results in the alignment of the lower extremities through the balance of ligaments in patients with severe genu valgus with pain reduction. , improvements in knee function and with a low rate of complications, the use of these alternatives such as the external approach in total knee replacement in patients with severe genu valgus and medial collateral ligament insufficiency allows correcting large deformities using a technique simple and in most cases without the use of a prosthesis that generates a degree of constraint, progressively improving their living conditions.
Keywords: Genu Valgus, Arthroplasty, Genu Varus
Angular Deformities (AD) of the lower limbs comprise a very common pathology in pediatric orthopedics. These can occur in relation to the frontal or sagittal plane. The DAs in the frontal plane are the Genu valgus and Genu varus. In the Genu valgus, the knee deviates inward from the midline, so that the lower extremities take on an “X” appearance. On the other hand, in the Genu varus, the knees deviate out of the midline and the extremities are arched in the form of a “parenthesis”.
In 90% of cases, these AD are typical of physiological development. The infant has a physiological Genu varus, disappearing by 2 years of age. From that moment, a contrary angulation begins, in Genu valgus (Figure 1), which reaches its maximum at 5 years and decreases until 7-8 years. Likewise, in adults a Genu valgus of 4-6º [1,2] is considered normal.
Among the main pathological causes are frequent metabolic alterations (hypophosphatemic rickets, renal osteodystrophy), skeletal dysplasia, traumatic sequelae, tumors, infections and idiopathic Genu valgus. They have also been associated with obesity [1,2].
Valgus deformities treated by knee replacement require a greater degree of surgical complexity. The correct ligament balance and the restoration of the gaps are fundamental objectives during the operative act and are essential to achieve a satisfactory result with long-term durability of the implant. In general, and in relation to the frequency of presentation, in the bibliography, there is a greater consensus on how to deal with a varus deformity, not so in valgus deformities, where there is no bibliography with a level of evidence that defines protocols established to treat severe valgus deformities>20º (Figure 2).
Total knee arthroplasty showed good clinical results in restoring lower limb alignment, reducing pain, and improving knee function in patients with moderate to severe knee osteoarthritis and genu valgus deformity. Postoperative coronal alignment is considered a prognostic factor for the clinical outcomes and survival rates of this surgery [3].
The instability of the tibio-femoral joint can occur in the coronal planes (Valgo). When performing a primary Total Knee Replacement (TKA), the use of an implant with increased stabilization (superior to a posterior stabilized prosthesis) is rare. This situation should be considered in knees in which it is not possible to achieve adequate stability through intraoperative soft tissue balance, due to partial or complete insufficiency of the collateral ligaments, especially the Medial Collateral Ligament (MCL) [4].
The severe Genu valgus (>20º) presents, with some frequency, some degree of insufficiency of the MCL, for which a standard implant might not be able to achieve a stable knee, especially in the medium term. The polyethylene plus prosthesis has a slightly taller and wider posterior stabilization post than the standard. These implants require sufficient collateral ligaments and represent only a small assistance in postoperative stability of the knee, which will continue to be dependent on the ligaments and other soft tissues [4,5].
Constrained implants have a higher and wider central post than the previous ones, in certain cases, with a central metal reinforcement that fits between the prosthetic femoral condyles of a femoral implant with a larger than standard drawer, which creates coronal and sagittal stability. These implants allow 2º or 3º axial and rotational movement, but the center post is not designed to withstand full loads of this type in the medium and long term. These implants have an acceptable medium-term survival, but very little is known about it beyond 10 years [4,5].
The external approach in total knee replacement is a useful surgical alternative for the management of patients with severe valgus deformity and medial collateral ligament insufficiency. It allows correcting large deformities without complex surgical procedures and using conventional implants without having to increase the degree of constraint.
The external approach described by Keblish allows, by means of a simple and reproducible surgical technique, to resolve cases of severe genu valgus without the need to use, in most cases, a prosthesis with an additional degree of constraint. In trained hands, this approach has a complication rate similar to that of other techniques.
A detailed bibliographic search of the required information is carried out that was published from 2016 to 2021, in the Scielo, Update, Medline, Pubmed, Elsevier databases, and the various national and international libraries. The following descriptors were used: Genu valgus, arthroplasty.
The data obtained oscillate between 7-15 records after the use of the different keywords, 8 articles were used for the realization of this document. The search for articles was carried out in Spanish and English, limited by year of publication, and studies published from 2014 to date that had information related to the external approach for Genu valgus knee arthroplasty were used.
Surgical management of valgus displacement of the knee is a controversial issue and there are even few reports in the updated literature. Although, in recent years, there has been an increase in published studies on this topic, the level of evidence still does not allow us to define an absolute management of these deformities. The most controversial questions in surgical treatment by arthroplasty in a patient with severe genu valgus and that still do not have conclusive answers, we could summarize them as: intra-surgical management of ligament balance (with its different technical options) and the need to use implants with constraint additional.
In a study carried out in Argentina and published in the journal of the Argentine Association of Orthopedics and Traumatology, 37 patients whose etiologies of deseje were: 3 cases of primary osteoarthritis with constitutional deseje (82.5%), four cases with a history of arthritis rheumatoid (10%), two patients with sequelae of tibial plateau fracture (5%) and one with sequelae of proximal tibial osteotomy (2.5%). After undergoing the surgical procedure using an external approach in knee arthroplasties with severe genu valgus, the radiographic measurements for correction of the misalignment were: mean preoperative femorotibial angle: valgus 27º (range 21-39) and average postoperative femorotibial angle: valgus 6, 2nd (range 4-10) [6].
 Figure 4:Bilateral genuine valgus. Patient operated on each knee 6 months apart. Previous valgus of 21° right and 24° left. Control in the office 4 months after surgery. Control radiographs at 10 months on the left and 4 months on the right.
Figure 4:Bilateral genuine valgus. Patient operated on each knee 6 months apart. Previous valgus of 21° right and 24° left. Control in the office 4 months after surgery. Control radiographs at 10 months on the left and 4 months on the right.Between 1997 and 2008, at the British Hospital in Buenos Aires, 681 primary RTRs were performed, of which 201 (29.5%) were performed in patients with genu valgus and developed a clinical-radiological classification system with the purpose of subdividing the sample according to the radiographic magnitude of the deseje and the degree of medial ligament sufficiency. Thus, three groups were determined:
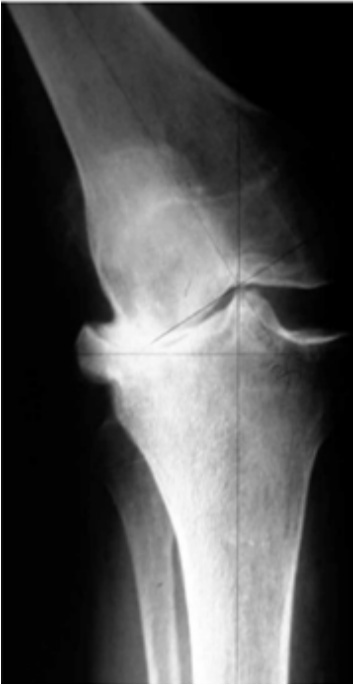 Figure 5: : Bilateral genuine valgus. Patient operated on each knee 6 months
apart. Previous valgus of 21° right and 24° left. Control in the office 4 months
after surgery. Control radiographs at 10 months on the left and 4 months on
the right.
Figure 5: : Bilateral genuine valgus. Patient operated on each knee 6 months
apart. Previous valgus of 21° right and 24° left. Control in the office 4 months
after surgery. Control radiographs at 10 months on the left and 4 months on
the right.Regarding the preoperative diagnosis, 26 (61.9%) had gonarthrosis; 10 (23.8%), rheumatoid arthritis; three, posttraumatic osteoarthritis and the remaining three were sequelae of overcorrected valgus femoral or tibial osteotomy. The 39 patients (42 KTRs) had a mean follow-up of 9.2 years (range 5 to 14.3). The Knee Society Score yielded an average preoperative value of 23.2 (range 17 to 38), while, postoperatively, it was 83.3 (range 70 to 92). Likewise, the Functional Knee Society Score was, on average, 27.5 (range 0 to 45) preoperatively and 82.5 (range 65 to 100) postoperatively.
The preoperative valgus angle of the series was, on average, 24.3º (range 21º to 45º). After the surgical procedure, the correction of said misalignment was achieved in almost all patients, an axis of between 3º and 8º was obtained in 88.1% of cases, with an average valgus angle of 5.9º (Figure 6) [7].
 Figure 6: : Bilateral genuine valgus. Patient operated on each knee 6 months apart. Previous valgus of 21° right and 24° left. Control in the office 4 months after surgery. Control radiographs at 10 months on the left and 4 months on
the right.
Figure 6: : Bilateral genuine valgus. Patient operated on each knee 6 months apart. Previous valgus of 21° right and 24° left. Control in the office 4 months after surgery. Control radiographs at 10 months on the left and 4 months on
the right.The results of this study show the benefit of external approach surgery in knee arthroplasty in patients with severe genu valgus; Taking into account a study carried out in Argentina, we can see the importance of treating soft tissues in the procedure, releasing and balancing soft tissues progressively, starting with the tenotomy of the fascia lata, the liberation of the ligament lateral collateral by means of the osteotomy of the external epicondyle and the section of the popliteal, only if necessary, and taking into account that in the genu valgus they affect the lateral collateral ligament, iliotibial band, popliteal tendon and posterolateral capsule, which is complicated by medial structures lax and incompetent for knee stability [7,8].
In an article published in the journal of the Argentine Association of Orthopedics and Traumatology, they show the effectiveness of arthroplasty for the management of genu valgus as a useful surgical alternative for the management of patients with severe valgus deformity and adequacy of the medial collateral ligament. It allows correcting large deformities without complex surgical procedures and using conventional implants without having to increase the degree of constraint and its results are comparable to those of other techniques, with a low rate of complications, but, above all, with the advantage of using primary implants no additional level of constraint [6].
Surgical treatment of valgus deviations of the knee is controversial, and there are even few reports in the up-to-date literature. Although there has been an increase in published research on this topic in recent years, the level of evidence still does not allow us to define the absolute management of these deformities. However, several studies have shown that the use of other alternatives such as the external approach in total knee replacement in patients with severe genu valgus and medial collateral ligament insufficiency allows correcting large deformities using a simple technique and in most cases without use of prostheses that generates a degree of constriction, where good results are evidenced in the alignment of the lower extremities through the balance of ligaments in patients with severe genu valgus with pain reduction, improvements in knee function with improvements to quality of life and low rates of complications
The author declares there is no conflicts of interest.
No funding.
1. Herrera M, Pais J (2017) Manual de patología quirúrgica del aparato locomotor. pp. 291–295.
2. https://riull.ull.es/xmlui/handle/915/20367.
3. Kim JG, Suh DH, Choi GW, et al. (2021) Change in the weight-bearing line ratio of the ankle joint and ankle joint line orientation after knee arthroplasty and high tibial osteotomy in patients with genu varum deformity. Int Orthop 45(1): pp. 117- 124.
4. Vedoya SP, Garabano G, del Sel H (2018) Indicación y resultados de la prótesis con estabilidad aumentada en la artroplastia primaria de rodilla [Constrained prosthesis primary total knee arthroplasty]. Revista de la Asociación Argentina de Ortopedia Traumatología 83(2): pp. 94-100.
5. Gehrke T, Kendoff D, Haasper C (2014) The role of hinges in primary total knee replacement. J Bone Joint Surg Br 96(11): pp. 93-95.
6. Silvano RE, Segura B, Torrecilla J, et al. (2021) Ventajas del abordaje externo para la artroplastia de rodilla por genu valgo severo. Rev Asoc Argent Ortop Traumatol 86(4): pp. 512-518.
7. Pesciallo C, Lopreite F, De Bielke H, et al. (2016) Artroplastia total de rodilla en genu valgo severo Seguimiento de 5 a 14 años. Rev Asoc Argent Ortop Traumatol 81(3): pp. 177-189.
8. Matehuala J (2018) Balance de tejidos blandos en la artroplastia total de rodilla. Orthotips 14(2): pp. 78-86.
PDF Google Scholar 10.52916/jmrs214061