 Journal of Medical Research and Surgery
PROVIDES A UNIQUE PLATFORM TO PUBLISH ORIGINAL RESEARCH AND REMODEL THE KNOWLEDGE IN THE AREA OF MEDICAL AND SURGERY
Journal of Medical Research and Surgery
PROVIDES A UNIQUE PLATFORM TO PUBLISH ORIGINAL RESEARCH AND REMODEL THE KNOWLEDGE IN THE AREA OF MEDICAL AND SURGERY
 Journal of Medical Research and Surgery
PROVIDES A UNIQUE PLATFORM TO PUBLISH ORIGINAL RESEARCH AND REMODEL THE KNOWLEDGE IN THE AREA OF MEDICAL AND SURGERY
Journal of Medical Research and Surgery
PROVIDES A UNIQUE PLATFORM TO PUBLISH ORIGINAL RESEARCH AND REMODEL THE KNOWLEDGE IN THE AREA OF MEDICAL AND SURGERY
 Indexed Articles
Indexed ArticlesSelect your language of interest to view the total content in your interested language
Anubha Bajaj*
Consultant Histopathologist, AB Diagnostics, India.
Correspondence to: Anubha Bajaj, Consultant Histopathologist, AB Diagnostics, India.
Received date: August 02, 2023; Accepted date: August 18, 2023; Published date: August 25, 2023
Citation: Bajaj A. The Autogenous Coelenterate-Endocervical Polyp Uterine Cervix. J Med Res Surg. 2023;4(4):84-85. doi: 10.52916/jmrs234115
Copyright: ©2023 Bajaj A. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted
use, distribution and reproduction in any medium, provided the original author and source are credited.
Endocervical polyp, Lesion, Epithelium, Chronic inflammation, Neoplasm.
Endocervical polyp represents as a benign, exophytic lesion constituted of variable admixture of proliferating endocervical glandular epithelium and metaplastic squamous epithelium permeated with a fibro-vascular core. The commonly encountered endocervical polyp is frequently accompanied by chronic inflammation, erosion of superficial epithelial surface and reactive alterations of layering epithelium.
Exceptionally, neoplasm may harbour foci of in situ or invasive squamous or glandular lesions of uterine cervix.
Generally, lesion is devoid of leaf-like architecture and periglandular stromal condensation, features which are pathognomonic of Müllerian adenosarcoma. The frequently discerned endocervical polyp represents in females exceeding >40 years although no age of disease emergence is exempt. Endocervical polyp represents as a non neoplastic lesion and commonly incriminates uterine cervix or endocervix.
Of obscure aetiology, chronic inflammation of uterine cervix is posited to induce endocervical polyp.
Endocervical polyp associated with microglandular hyperplasia or polypoid cervical microglandular hyperplasia may be associated with gestation or influences of exogenous progestin administration. Majority of endocervical polyps are discovered incidentally upon a routine gynaecological examination. Neoplasm may represent with abnormal vaginal spotting or bleeding, postcoital bleeding, anomalous vaginal discharge or bleeding on contact.
Grossly, endocervical polyp manifests as a singular lesion. Frequently, tumefaction represents with a magnitude <1 centimetre.
Upon frozen section examination, endocervical polyp demonstrates a morphology akin to features encountered upon permanent, formalin fixed, paraffin embedded sections. Upon frozen section, segregation from neoplasms as adenosarcoma is necessitated. In contrast to adenosarcoma, endocervical polyp appears devoid of condensation of periglandular stroma or papillary, intra-glandular projections. Stromal or epithelial cell atypia is absent.
Upon microscopy, endocervical polyp depicts a fibrovascular core pervaded with vascular articulations of variable magnitude. Generally, thick walled arterial configurations are expounded. Intervening stroma is variably cellular and admixed with chronic inflammatory cell infiltrate. Surface epithelium represents as endocervical glandular subtype with foci of squamous metaplasia, cervical erosion and reactive or reparative alterations within uterine cervix. Proliferation of endocervical glands may ensue with concordant cystic alterations or with occurrence of benign microglandular hyperplasia. Mitotic activity is significant, especially within lesion delineating prominent inflammation or florid microglandular hyperplasia.
Epidermal metaplasia may occur along with demonstration of cutaneous appendage structures. Stromal cells may be multinucleated, demonstrate focal decidual alterations demonstrate heterologous elements as adipose tissue, cartilage, bone or glial tissue, possibly representing retained foetal tissues from preceding gestation. Exceptionally, endocervical polyp may harbour foci of in situ or invasive squamous or glandular lesions, as denominated by High Grade Squamous Intraepithelial Lesion (HSIL), adenocarcinoma in situ, squamous cell carcinoma or adenocarcinoma [1-5] (Figure 1 and 2).
TNM staging of carcinoma cervix 2021 as per American Joint Committee on Cancer (version 9) [3,4].
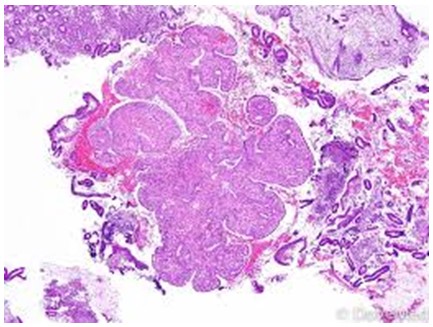 Figure 1: Endocervical polyp demonstrating proliferating glandular epithelium and metaplastic epithelium inundated with a fibro-vascular core. Surrounding stroma is fibrotic, cellular and imbued with chronic inflammatory cells [6].
Figure 1: Endocervical polyp demonstrating proliferating glandular epithelium and metaplastic epithelium inundated with a fibro-vascular core. Surrounding stroma is fibrotic, cellular and imbued with chronic inflammatory cells [6].
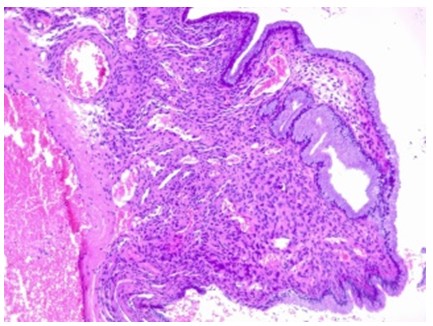 Figure 2: Endocervical polyp exhibiting proliferating glandular epithelium and metaplastic squamous epithelium incorporated with a fibro-vascular core. Encompassing stroma is cellular, fibrotic and infiltrated with chronic inflammatory cells [7].
Figure 2: Endocervical polyp exhibiting proliferating glandular epithelium and metaplastic squamous epithelium incorporated with a fibro-vascular core. Encompassing stroma is cellular, fibrotic and infiltrated with chronic inflammatory cells [7].
Generally, immunohistochemistry appears superfluous in discerning endocervical polyp. Epithelial component appears immune reactive to diverse epithelial markers as cytokeratin or Epithelial Membrane Antigen (EMA). Stromal component appears immune reactive to vimentin and diverse smooth muscle markers.
Endocervical polyp appears immune non reactive to p16, in contrast to High Grade Squamous Intraepithelial Lesion (HSIL) or adenocarcinoma in situ. Endocervical polyp of uterine cervix requires segregation from neoplasms such as adenosarcoma, endometrial polyp, polypoid adenomyoma or condyloma. Besides, abnormal uterine bleeding engendered by endocervical polyp necessitates demarcation from lesions such as uterine fibroid, endometrial hyperplasia, endometrial carcinoma, endometriosis, adenomyosis, cervical ectropion, carcinoma cervix, surface lesions of the genital tract, Sexually Transmitted Infections (STIs), conditions related to gravid uterus as ectopic pregnancy or an endometrial polyp projecting through cervical canal. Endocervical polyp appears to protrude through external os of the cervical canal and may be discerned upon routine gynaecologic examination or colposcopy.
Cervical smears stained with Papanicolaou stain may exhibit atypical cells occurring due to reactive epithelial alterations confined to the surface.Endocervical polyp can be optimally treated with surgical manoeuvers as polypectomy which is recommended for alleviating symptomatic polyps or enlarged endocervical polyps >3 centimetre magnitude.
Excision of endocervical polyps during gestation may be challenging. Enhanced possible occurrence of pregnancy loss and preterm birth may ensue subsequent to endocervical polypectomy adopted as a therapeutic strategy within pregnant women.
The authors have no conflicts of interest to report.
No
