 Journal of Medical Research and Surgery
PROVIDES A UNIQUE PLATFORM TO PUBLISH ORIGINAL RESEARCH AND REMODEL THE KNOWLEDGE IN THE AREA OF MEDICAL AND SURGERY
Journal of Medical Research and Surgery
PROVIDES A UNIQUE PLATFORM TO PUBLISH ORIGINAL RESEARCH AND REMODEL THE KNOWLEDGE IN THE AREA OF MEDICAL AND SURGERY
 Journal of Medical Research and Surgery
PROVIDES A UNIQUE PLATFORM TO PUBLISH ORIGINAL RESEARCH AND REMODEL THE KNOWLEDGE IN THE AREA OF MEDICAL AND SURGERY
Journal of Medical Research and Surgery
PROVIDES A UNIQUE PLATFORM TO PUBLISH ORIGINAL RESEARCH AND REMODEL THE KNOWLEDGE IN THE AREA OF MEDICAL AND SURGERY
 Indexed Articles
Indexed ArticlesSelect your language of interest to view the total content in your interested language
Mouhamadou Mansour Niang1,2*, Fatou Samb2, Cheikh Tidiane Cisse1,2
1Département of Obstetrics and Gynecology, Cheikh Anta Diop University of Dakar, Senegal
2Département of Obstetrics and Gynecology, Hospital Institute of Social Hygiene, Senegal
Correspondence to: Mouhamadou Mansour Niang, Associate Professor in Gynecology-Obstetrics, Department of Gynecology-Obstetrics, Hospital Institute of Social Hygiene of Dakar, Senegal
Received date: July 14, 2022; Accepted date: August 02, 2022; Published date: August 09, 2022
Citation: : Niang MM, Samb F, Cisse CT. Subacute Non-Puerperal Uterine Inversion: A Rare Complication of Uterine Myoma. J Med Res Surg. 2022; 3(S2): 1-3. doi: 10.52916/jmrs22S201
Copyright: ©2022 Niang MM, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted
use, distribution and reproduction in any medium, provided the original author and source are credited.
Subacute non-puerperal uterine inversion is an extremely rare clinical situation that constitutes a medico-surgical emergency that can be life-threatening for women due to the risk of bleeding. We report the case of a 45 years-old patient, second parous received urgently with hemorrhagic shock. The clinical examination confirmed the diagnosis of uterine inversion secondary to a fundic myoma type 0 delivered through the cervix. Resuscitation was carried out followed by surgical management by a mixed vaginal and abdominal approach to perform a hysterectomy. Through this clinical case, we recall the epidemiological aspects of this pathology as well as the diagnostic and therapeutic difficulties.
Non puerperal uterine inversion, Submucosal fibroid, Hysterectomy
Uterine inversion or “uterine intussusception” occurs when the uterine fundus collapses into the endometrial cavity, turning the uterus partially or completely inside out. Several degrees have been described ranging from simple depression of the uterine fundus (1st degree) to its complete exteriorization outside the vulva (4th degree). This is an extremely rare clinical situation, most often occurring in postpartum even if the gynecological origin is possible. Indeed, in France, its frequency is estimated at 1/100,000 deliveries, 85% of which are puerperal uterine inversion. Its severity is linked to the risk of hemorrhagic shock that can be life-threatening for women [1]. Our objective was to report this case of non-puerperal uterine inversion secondary to a type 0 uterine myoma delivered through the cervix and to discuss the epidemiological aspects and the diagnostic and therapeutic difficulties related to this pathology.
Ms. KS, 45 years old, a second parous with two living children born vaginally, was received in the emergency room with a genital bleeding complicated by consciousness disorders. The interrogation finds a notion of menometrorrhagia and secondary infertility since 8 years. The general examination found clinical anemia and a state of cardiovascular collapse with blood pressure at 90/50 mmHg and an accelerated pulse at 120 beats per minute. Resuscitation was carried out immediately with vascular filling using fluids and mask oxygenation to obtain hemodynamic stability. The vulvo-perineal inspection found a genital haemorrhage associated with the presence of a fleshy extra-vulvar mass of approximately 8cm in long axis surmounted by the uterine body with areas of necrosis (Figure 1).
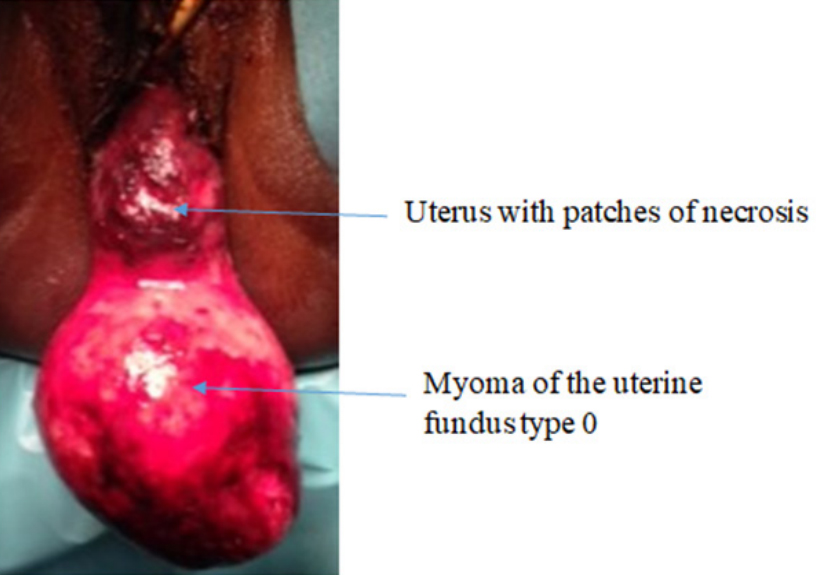 Figure 1: Third degree uterine inversion secondary to a myoma of the uterine
fundus (Picture Ouakam Military Hospital).
Figure 1: Third degree uterine inversion secondary to a myoma of the uterine
fundus (Picture Ouakam Military Hospital).The complete blood count revealed severe anemia with a hemoglobin level of 6 g/dL. The diagnosis of uterine inversion of the 3rd degree complicated by severe anemia was suspected and confirmed by a trans-abdominal pelvic ultrasound which did not find the uterus in the pelvic cavity.
The patient received an isoRhesus isogroup whole blood transfusion. Surgical excision of the myoma under general anesthesia was performed via the vagina followed by a futile attempt to reintegrate the uterine fundus due to the cervical pinch ring. The decision of a laparotomy was taken and made it possible to objectify an absence of uterus with in its place a central-pelvic depression attracting the two ovaries, the fallopian tubes and the round ligaments (Figure 2).
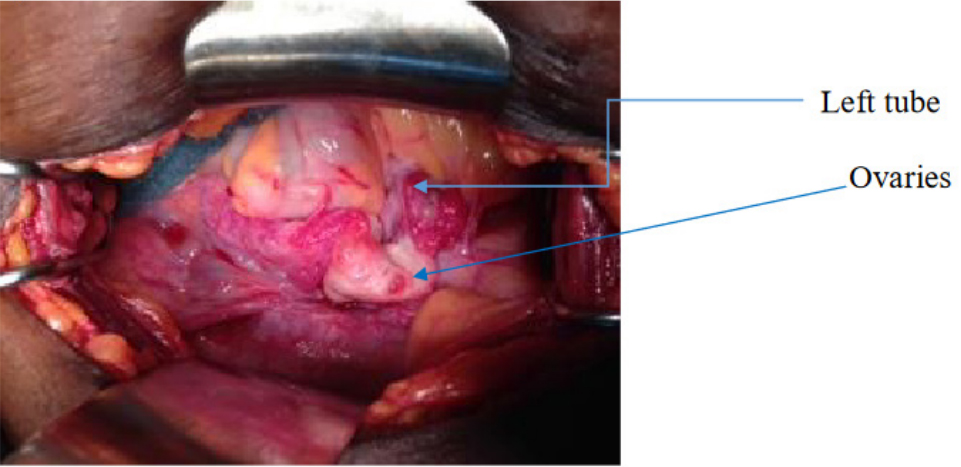 Figure 2: Central-pelvic depression attracting the tubes and the ovaries
(Picture Ouakam Military Hospital).
Figure 2: Central-pelvic depression attracting the tubes and the ovaries
(Picture Ouakam Military Hospital).The indication of a hysterectomy was taken. We began the operation with the ligation and the section of the round ligament through the abdomen and a posterior section of the cervical pinch ring through the vagina. This allowed a better mobilization of the uterus and the realization of the total hysterectomy with bilateral adnexectomy. There were no postoperative complications and the patient was discharged on the 3rd day after the surgery. The histological analasis of the surgical specimen revealed a uterine leiomyoma.
Uterine inversion is a serious medical and surgical emergency because it can be life-threatening for women. It is most often of obstetrical origin. Its frequency is highly variable depending on the studies, ranging from 1/20,000 to 1/2,500 deliveries [2]. Non-puerperal uterine inversion is rare with less than 200 cases reported in the literature [3]. Four anatomo-clinical stages have been described [4]:
We speak of an acute inversion when it is discovered within 30 minutes. Beyond that, cervical edema forms, forming a ring hindering the reintegration of the uterine body: this is then a sub-acute inversion. A chronic inversion being defined by its discovery more than 30 days after its constitution [5].
Non-puerperal uterine inversion generally occurs in postmenopausal women or over 45 years [6], as was the case with our patient. Indeed, its occurrence requires uterine hypotonia and sufficient cervical dilation found especially in multiparous women. Our patient was a second parous and the type 0 myoma due to its size caused a distension of the uterine cavity and an opening of the cervix favorable to the expulsion of the myoma and the occurrence of the uterine inversion. Several factors are involved in the pathophysiology of non-puerperal uterine inversion, in particular the presence of a uterine tumor located preferentially on the uterine fundus, on a thin uterine wall, with a small tumor pedicle, rapid tumor growth and cervical dilation. by distension of the uterine cavity [7].
The diagnosis of uterine inversion is clinical with, in the acute and subacute forms, intense pelvic pain associated with metrorrhagia and the appearance of a vaginal or extravulvar mass [8]. Our patient was received in an array of cardiovascular collapse secondary to uterine bleeding. Non-puerperal etiologies are dominated by endocavitary tumours, most often benign such as uterine myoma (70 to 85%) or sometimes malignant (15 to 30%) such as leiomyosarcoma, embryonal rhabdomyosarcoma and endometrial stromal sarcoma. In the case of our patient, the uterine inversion was secondary to a large type 0 myoma for which implantation base extended over the entire uterine fundus. The management of uterine inversion combines effective resuscitation and conservative (reintegration of the uterus into the pelvic cavity) or radical (hysterectomy) surgical treatment. In our patient, we opted for a radical treatment taking into account her age, the severity of the clinical case and the appearance of the uterus, in particular the presence of areas of necrosis. The approach was mixed (vaginal and abdominal) as recommended by most of the authors [9]. It makes it possible to minimize the technical difficulties due to the modifications of the usual anatomical landmarks, in particular the excretory urinary tracts (ureters and bladder). We performed the myomectomy via the vagina followed by the section of the cervical pinch ring. Via the abdominal route, we proceeded to the ligature-section of the uterine ligaments. These gestures made possible the replacement of the uterus in the pelvis and the continuation of the hysterectomy through the abdominal route. The same surgical technique has been reported in the literature [10-12].
Uterine inversion is a medico-surgical emergency most often of puerperal origin. Non-puerperal etiologies are often submucosal myoma. Its severity is related in the risk of haemorrhagic shock that can be life-threatening for the woman. In the absence of a desire for pregnancy, total hysterectomy by a mixed abdominal and vaginal route is the treatment of choice and allows to avoid technical difficulties and reduce operative complications.
The authors have no known conflict of interest to disclose.
None.
