 Journal of Medical Research and Surgery
PROVIDES A UNIQUE PLATFORM TO PUBLISH ORIGINAL RESEARCH AND REMODEL THE KNOWLEDGE IN THE AREA OF MEDICAL AND SURGERY
Journal of Medical Research and Surgery
PROVIDES A UNIQUE PLATFORM TO PUBLISH ORIGINAL RESEARCH AND REMODEL THE KNOWLEDGE IN THE AREA OF MEDICAL AND SURGERY
 Journal of Medical Research and Surgery
PROVIDES A UNIQUE PLATFORM TO PUBLISH ORIGINAL RESEARCH AND REMODEL THE KNOWLEDGE IN THE AREA OF MEDICAL AND SURGERY
Journal of Medical Research and Surgery
PROVIDES A UNIQUE PLATFORM TO PUBLISH ORIGINAL RESEARCH AND REMODEL THE KNOWLEDGE IN THE AREA OF MEDICAL AND SURGERY
 Indexed Articles
Indexed ArticlesSelect your language of interest to view the total content in your interested language
Yogesh Sharad Salphale1* , Gopal Mahadeo Shinde2, Atharva Rajesh Sharma3, Piyush Gadegone1, Wasudeo Gadegone1
, Gopal Mahadeo Shinde2, Atharva Rajesh Sharma3, Piyush Gadegone1, Wasudeo Gadegone1
1Consultant Orthopaedic Surgeon, Shushrusha Multispecialty Hospital, Lane Opp. Z.P, Chandrapur, Maharashtra, India
2Associate Professor, Department of Orthopaedics, Maharashtra Post Graduate Institute of Medical Education and Research , Maharashtra University of Health Sciences, Nashik, Maharashtra, India
3Junior Resident, HBT Medical College And Dr. R N Cooper Hospital, Juhu, Mumbai, Maharashtra, India
Correspondence to: Yogesh Sharad Salphale, Consultant Orthopaedic Surgeon, Shushrusha Multispecialty Hospital, Lane Opp. Z.P, Chandrapur, Maharashtra, India
Received date: March 03, 2023; Accepted date: March 15, 2023; Published date: March 22, 2023
Citation: Salphale YS, Shinde GM, Sharma AR, et al. Retrograde Intramedullary Interlocking Nailing in Fractures of the Distal Femur: A Review of 20 Cases with an Average Follow-Up of One Year. J Med Res Surg. 2023;4(2):27-30. doi: 10.52916/jmrs234102
Copyright: ©2023 Salphale YS, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted
use, distribution and reproduction in any medium, provided the original author and source are credited.
Objectives: In patients with distal femur fractures, we studied the role of retrograde locked intramedullary nails.
Methods: Retrograde locked intramedullary nailing was used to treat the distal femur fractures of 20 patients (15 males, 5 females; mean age 47 years; range 25 to 69 years). Two patients had fracture of the distal femur and shaft. The fractures were classified as A1 (n=12), A2 (n=6), A3 (n=2), by the AO classification. There were two Grade I open fractures and 18 closed fractures. Three fractures were managed with percutaneous technique. At the mean first follow-up time of 18 months (range 15-48 months and mean second follow up at 27 months (range 12 to 68 months), the concluding functional results were assessed by using the modified Hospital for Special Surgery (HSS) knee assessment scale.
Results: The average time to achieve union was 24.2 weeks (range 14 to 42 weeks). One patient had a delayed union (44 weeks). Five knees (25%) had normal joint range of motion, ten knees (50%) were having range of motion from 100° to 110°, three knees (15%) were having range of motion of 80°, and two knees (10%) were having range of motion below the 80°. According to the modified HSS knee scale, the results were excellent in eleven cases (55%), good in six (30%), moderate in two (10%), and poor in one case (5%). In two patients (10%), the postoperative radiographic examination revealed varus angulation (10°), healing took place with severe distortion in one subject. None of the patient had any deep infection or wound issues.
Conclusion: Retrograde femoral nailing is an effective method for treating distal femoral shaft fractures. The healing rate of femoral shaft fractures fixed with a retrograde nail is the same regardless of fracture location, patient age, gender, or degree of comminution. For good results surgical treatment, post-surgery immediate knee mobilisation and avoiding nail tip prominence in the knee are essential.
Distal femur fracture, Retrograde nailing, Knee pain, Knee injury ondylar nailing, Knee fracture
The distal portion of the femur accounts for around 6% of all fractures. The methods and implants used to treat femoral shaft fractures have changed over time. One of these was the use of an antegrade interlocking intramedullary nail, which was regarded as the gold standard. Because of the greater shaft diameter, the ability to adjust antegrade nailing in the distal diaphyseal femoral fractures have been regarded to be difficult to manage [1-4]. However, every method and implant have some restrictions. Due to antegrade nailing's limitations when distal femoral fractures were considered, retrograde nailing for distal femoral shaft fractures came in vogue. Due to the reaming, surgical dissection, and fracture in the distal portion, this method frequently results in knee pain. An apparent risk factor for knee pain was younger age. For distal femoral shaft fractures treated with either retrograde nailing or plating, no statistically significant difference in knee discomfort or knee movement was noted [5].
The present retrospective study was conducted in the Department of Orthopaedics at our Institute and included 20 patients who were treated from January 2016 to December 2019 (15 males, 5 females; mean age 47 years; range 25 to 69 years). Two patients had fracture of the distal femur and shaft. The fractures were classified as A1 (n=12), A2 (n=6), A3 (n=2), by the AO classification (Figure 1). There were two Grade I open fractures and 18 closed fractures. Three fractures were managed with percutaneous technique. Patients with prior knee surgery or intervention, as determined by medical records, symptoms of an infection (purulent discharge), advanced osteoarthritis of the knee joint, as determined by an X-ray showing osteophytes and reduced joint space, any history of connective tissue disorders were excluded from this study. Before deciding on a surgical fixation strategy for distal femur fractures, radiographs were taken in two planes: the anteroposterior view and the lateral view.
The affected knee was positioned over the operating table with the patient lying supine and a bolster underneath it to achieve an angle upto 30 degrees. Knee flexion prevents the gastrocnemius from pulling the distal fragment into further flexion. Borders of the patella tendon and inferior pole of the patella were marked. An incision was made at the inferior pole of the patella and entry portal made through the patellar tendon. The intercondylar notch's centre served as the starting point for the guide pin. After seeing the lateral view, and a anteroposterior view, the entry point was taken just superior to Blumensaat's line as seen on a C-arm lateral image. The fracture was reduced and the nail entry portal was enlarged. A guidewire was passed from the entry portal inside the medullary canal and the entry portal was widened judiciously to accommodate the nail. The nail of adequate length and diameter was implanted with gentle movements which was then locked distally and proximally (Figure 2). Care was taken to avoid the nail being proud inside the knee joint. After the implants were placed they were locked proximally and distally. The knee joint was thoroughly lavaged and the closure was performed in the routine manner. Care was taken to assess the knee ligament injuries after proximal and distal interlocking and the hip was visualised before the patient was shifted out of the Operating Room (OR).
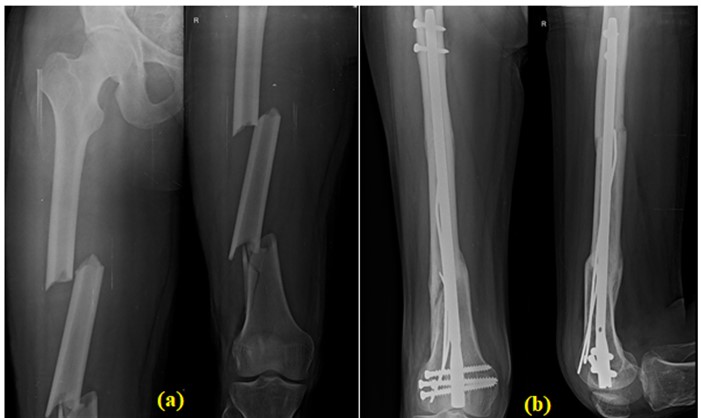 Figure 2: (a): Showing a segmental fracture of the femur with communition;
(b): shows a well healed fracture with well healed callus, supplementary
nails and additional screws to impart stability in distal femur.
Figure 2: (a): Showing a segmental fracture of the femur with communition;
(b): shows a well healed fracture with well healed callus, supplementary
nails and additional screws to impart stability in distal femur.In our study of the distal femur fractures of 20 patients there were 15 males and 5 females. Their age ranged from 25 to 69 years with the mean age 47 years. 13 patients had Roadside Accident (RSA) as mode of trauma for their fracture and 7 patients had a domestic fall. There were two Grade I open fractures and 18 closed fractures. Two patients had fracture of the distal femur and shaft. Three fractures were managed with percutaneous technique and passage of additional nails to compensate for the void in the medullary canal (Figure 1). Mean operating time was 60 ± 10 minutes. Mean blood loss was approximately 80 ml. The average time to achieve union was 24.2 weeks (range 14 to 42 weeks). One had a delayed union (44 weeks). Five knees (25%) had normal joint range of motion, ten knees (50%) were in the 100 to 110° range, three knees (15%) were in the 80° range, and two knees were below the 80° mark (10 %). At the conclusion of a mean follow-up time of 18 months (range 15-48 months), functional results were assessed using the modified Hospital for Special Surgery (HSS) knee assessment scale.
The results were excellent in eleven femurs (55%), good in six (30%), moderate in two, (10%) and poor in one femur (5%), according to the modified HSS knee scale in two patients (10%), the postoperative radiographic examination revealed varus angulation (10°). Healing took place with severe distortion in one subject aged 62 yrs but that did not affect the functional outcome (Figure 3). None of the patient had any deep infection or wound issues.
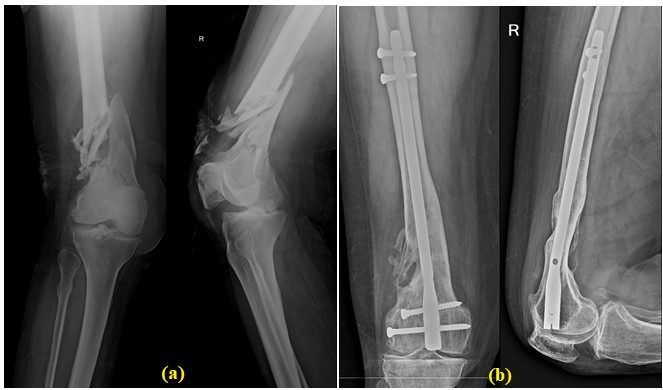 Figure 3: (a): Commnuited fracture of the distal end of the femur in a 65
year old lady; (b): Commnuited fracture of the distal end of the femur healed
well.
Figure 3: (a): Commnuited fracture of the distal end of the femur in a 65
year old lady; (b): Commnuited fracture of the distal end of the femur healed
well.Between 4% to 6% of femoral fractures and roughly 0.4% of adult fractures are distal femur fractures [6]. Distal femur fractures often affect one of two populations: either younger persons who have experienced high-energy trauma or elderly people, primarily women with osteoporotic bones. The ease of retrograde nail insertion, its applicability to polytrauma patients, patients with ipsilateral femoral neck and shaft fractures, and patients with multiple fractures, to name a few, are just a few of the potential benefits of retrograde IM nailing of femoral shaft fractures [7,8].
With interlocking screws applied in the distal segment, retrograde nailing can achieve a relatively longer working length and improve fracture stability. Retrograde nailing is known to provide an advantage over antegrade nailing for below-isthmus femoral shaft fractures in terms of implant insertion, control of the short distal segment, and fixation strength [9,10] despite concerns of articular cartilage damage and postoperative knee pain. The retrograde femur geometry at its insertion end is more congruous for achieving the acceptable anatomical reduction at the fracture site in supracondylar region of the femur, thus causing less chances of the nonunion/delayed union as compared to the antegrade nailing. When retrograde nailing is being done, the patient is positioned supine, which gives the surgeon more fluoroscopic control over the greater trochanter and better axis control. Retrograde nailing is technically simpler in obese patients or patients with multiple fractures, thus making it easier to access other fractures, and eliminates the need for a traction table [11]. The possible reduction of intraoperative patient manipulation, which would reduce overall surgical time for patients with numerous injuries, is a significant benefit [12,13].
Antegrade nailing was once believed to be "problem free," but recent research has shown that it is frequently linked to trochanteric pain (40%), thigh pain (10%), stiffness (38%), limp (13%), decreased walking distance (12.5%), and difficulty climbing stairs (10%), postoperative pudendal nerve palsy reported to be as high as 15% [14,15] and functionally significant heterotopic ossification around the hip. There is no doubt that the insertion of any IM implant should begin at the long axis of the medullary canal [16,17]. We agree that the risk of impaired knee function is unfound, with low incidence of pain and limping [18,19].
In our series, the nail neither reach the subtrochanteric level or the nails allowed us for the multidirectional locking. The nails we used for the study had an option of latero-medial locking in the proximal and distal end. Despite the large number of fractures in this series being stabilized with a nail not reaching in the subtrochanteric region, no implant failures occurred. In the Centre like ours, where there was no dedicated physiotherapist, patients were from rural region and were not asked to follow the challenging rehabilitation protocol. Still there was no implant failure which we feel could be attributed to the cautious mobilization protocol.
Up to 70%, postoperative knee pain has been associated with retrograde nailing. Possible reasons of this pain include quadriceps atrophy, distal locking screws, concomitant patellar or ligamentous injury, original trauma, infections of the knee joint, and projecting nails [20]. Stable fractures deprived of axial loading by static locking in distraction or prolonged non-weight bearing, appear to be at risk for impaired fracture healing.The current designs with multiple holes in the lateral and anteroposterior directions allow the placement of locking screws in different planes and contribute to the mounting stability. Using a split patellar tendon and intercondylar distal femoral entry portal, our findings suggest that unreamed retrograde IM nailing of femoral shaft fractures is quick and easy,has little blood loss and can produce outcomes that are comparable to those of reamed antegrade nailing.
Unreamed retrograde nailing is presented as a secure and advantageous fracture fixation technique that should be added to the orthopaedic surgeon's armamentarium, though it is not recommended as a replacement for other methods. Further study is warranted to evaluate its applicability for patients with isolated injury, the long-term effect on knee function, and the potential for improved functional outcome as compared with reamed antegrade nailing.
We have no known conflict of interest to disclose.
No
