 Journal of Medical Research and Surgery
PROVIDES A UNIQUE PLATFORM TO PUBLISH ORIGINAL RESEARCH AND REMODEL THE KNOWLEDGE IN THE AREA OF MEDICAL AND SURGERY
Journal of Medical Research and Surgery
PROVIDES A UNIQUE PLATFORM TO PUBLISH ORIGINAL RESEARCH AND REMODEL THE KNOWLEDGE IN THE AREA OF MEDICAL AND SURGERY
 Journal of Medical Research and Surgery
PROVIDES A UNIQUE PLATFORM TO PUBLISH ORIGINAL RESEARCH AND REMODEL THE KNOWLEDGE IN THE AREA OF MEDICAL AND SURGERY
Journal of Medical Research and Surgery
PROVIDES A UNIQUE PLATFORM TO PUBLISH ORIGINAL RESEARCH AND REMODEL THE KNOWLEDGE IN THE AREA OF MEDICAL AND SURGERY
 Indexed Articles
Indexed ArticlesSelect your language of interest to view the total content in your interested language
Nimra Ali* , Danial Khalid, Muhammed Ali, Raisa Altaf, Uzma, Ramsha Fatima Qureshi
, Danial Khalid, Muhammed Ali, Raisa Altaf, Uzma, Ramsha Fatima Qureshi
Department of Radiology, Liaquat National Hospital and Medical College, Karachi, Pakistan.
Correspondence to: Nimra Ali, Department of Radiology, Liaquat National Hospital and Medical College, Karachi, Pakistan.
Received date: April 04, 2023; Accepted date: April 25, 2023; Published date: May 02, 2023
Citation: Ali N, Khalid D, Ali M, et al. Pulmonary Artery Aneurysm: A Rare Case Report. J Med Res Surg. 2023;4(2):31-32. doi: 10.52916/jmrs234103
Copyright: ©2023 Ali N, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted
use, distribution and reproduction in any medium, provided the original author and source are credited.
Pulmonary artery aneurysm is a rare entity involving aneurysmal dilatation of the main pulmonary artery. It is associated with structural cardiac anomalies, structural vascular abnormalities, pulmonary artery hypertension, vasculitis and infection. In some cases, it can also be idiopathic. Clinical presentation may vary in different patients and are nonspecific. Treatment is usually surgical intervention once diagnosed. We have presented one such case of a patient whose Computed Tomography (CT) scan showed a large aneurysm of descending branch of pulmonary artery.
Pulmonary artery, Anomalies, Aneurysmal dilatation, Surgical intervention
Aneurysm of the pulmonary artery is rarely reported. It may be associated with congenital as well as acquired conditions. Rarely it is reported as idiopathic. It is defined as the focal dilatation of pulmonary artery. Normal main pulmonary artery measures 29 mm and inter lobar artery measures 17 mm on CT [1-3]. All three layers of the vascular wall-the tunica intima, tunica medium, and tunica adventitia-must be involved for an artery to be considered to have an actual aneurysm. Contrarily, a pseudoaneurysm does not involve each of the three layers and as a result, is more likely to rupture [3].Clinical manifestations are nonspecific and patient may present with hemoptysis, shortness of breath, chest pain, palpitation, cough or fever [1-3]. Pulmonary angiography is gold standard in diagnosing Pulmonary Artery Aneurysms (PAA) however other modalities can be useful such as CT scan, Magnetic Resonance Imaging (MRI) or Echocardiogram (ECHO). Treatment is controversial, the main treatment strategies include surgical intervention or angioembolization, however surgical intervention is recommended to avoid rupture or dissection in large sized aneurysms.
A 60 year old female known case of Diabetes Mellitus (DM) and Chronic Kidney Disease (CKD) presented to the Emergency Department of our hospital with cough, fever and shortness of breath. She was vitally unstable with SPO2 of 82%, RR=30 breath/min, her neurological and abdominal examination was unremarkable. She was advised a CT chest which showed a large aneurysm of descending branch of pulmonary artery which measured about 4.6 × 7.0 × 7.9 cm (AP × TS × CC). blush of contrast was also seen. Patient had an uneventful recovery and was discharged from the hospital.
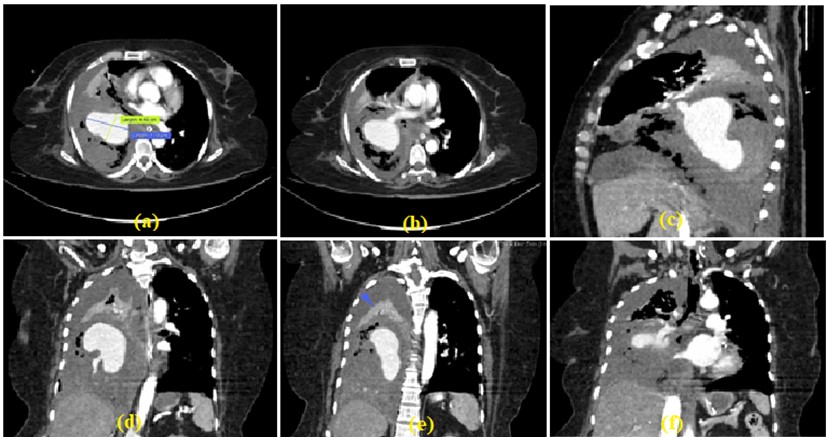 Figure 1 (a-f): Axial, coronal and sagittal images of CT scan chest show a large aneurysm of descending branch of pulmonary artery.
Figure 1 (a-f): Axial, coronal and sagittal images of CT scan chest show a large aneurysm of descending branch of pulmonary artery.Pulmonary artery aneurysm is a rare presentation with an incidence rate of 1 in 14000 autopsies [2,3]. The natural history is not fully known, and there are no established rules on the surgical indications (the relationship between the size of the PAA, its location, and the risk of rupture is not as clearly defined as for aortic aneurysms) [4]. It is associated with several congenital as well as acquired conditions like structural cardiac and vascular anomalies, connective tissue disorders, infection, pulmonary artery hypertension and vasculitis are common [1,2]. In general, acquired aetiologies such trauma, iatrogenic damage, infection, and behcet's disease are responsible for the majority of PAA cases [3]. Among the congenital problems may involve intracardiac shunting, right ventricular outflow tract blockage, tricuspid valve disease in intravenous drug users, vascular abnormalities such arteritis, and Pulmonary Arterial (PA) hypertension [5]. For an artery to be classified as having a genuine aneurysm, all three layers of the vascular wall-the tunica intima, tunica medium, and tunica adventitia-must be affected. A pseudoaneurysm, on the other hand, does not involve all three layers and is hence more susceptible to rupture [3]. Idiopathic aneurysm occurs rarely [1,2]. These entities were separated into those with and without an arterio-venous connectivity according to a suggested categorization of PAAs [4]. An enlarged pulmonary trunk detected on a chest radiogram requires consideration of a PA aneurysm as part of the differential diagnosis; two-dimensional echocardiography should be done first [6].
However, our patient had no association with the above mentioned anomalies. Clinical presentation of PAA is non-specific however patients with PAA may often experience hemoptysis, dyspnea with exertion, fever or cough, and chest pain [1-3,7]. Our patient also presented with cough, fever and dyspnea. The diagnosis is made using a chest X-ray, CT scan, digitalized pulmonary angiography, and echocardiography, which also aid in determining extension and location [8]. The gold standard for the diagnosis of PAAs is pulmonary angiography but other modalities have replaced angiography for the diagnosis of PAA as a result of recent technology advancements that include echocardiography, both transthoracic and trans-esophageal, and magnetic resonance imaging or CT [1,2,7]. Our patient also had her CT chest done that showed a large aneurysm of descending branch of right pulmonary artery. It is recommended that large aneurysms of >6 cm and those that are symptomatic of any size should be repaired [3,9]. For management, there are no precise rules. When there was no left-to-right intracardiac shunt or severe pulmonary arterial hypertension, conservative therapy was advised. This led to a generally benign prognosis with a simple course after 1 to 7 years of follow-up [9]. In non-urgent, asymptomatic patients, conservative management of a PAA can be considered to address treatable underlying etiologies [1,3,9]. If the patient has a tolerably low operational risk, surgical therapy should be taken into account for big pulmonary trunk aneurysms regardless of their underlying cause or condition [10]. The surgical techniques that have been described include aneurysmorrhaphy or arterioplasty, pericardial patch reconstruction, and interposition grafting with allografts or synthetic textile grafts as treatment methods for aneurysms of the main PA [1,2,5,9]. Steel coil embolization has recently shown promising results for treatment of peripheral PAAs [1]. It is widely accepted minimally invasive therapy. Intra-saccular embolization with coils has the advantage of preserving the pulmonary arteries distal to a PAA or PAPA [3]. In our patient, coil embolization was done to occlude the neck of aneurysm. Post emboilization angiogram showed near complete occlusion of the aneurysm. The outcome of the procedure was successful and patient was moved to the primary ward.
Aneurysm of pulmonary artery are uncommon yet an important diagnosis. The diagnosis is crucial to save the patient from significant mortality. We have therefore presented this case to help radiologist in quick diagnosis of such cases. If the patient has an acceptable low operational risk, surgical therapy should be taken into account for big pulmonary trunk aneurysms regardless of their aetiology and underlying illness to prevent a potential rupture with deadly results.
We have no known conflict of interest to disclose.
No
