 Journal of Medical Research and Surgery
PROVIDES A UNIQUE PLATFORM TO PUBLISH ORIGINAL RESEARCH AND REMODEL THE KNOWLEDGE IN THE AREA OF MEDICAL AND SURGERY
Journal of Medical Research and Surgery
PROVIDES A UNIQUE PLATFORM TO PUBLISH ORIGINAL RESEARCH AND REMODEL THE KNOWLEDGE IN THE AREA OF MEDICAL AND SURGERY
 Journal of Medical Research and Surgery
PROVIDES A UNIQUE PLATFORM TO PUBLISH ORIGINAL RESEARCH AND REMODEL THE KNOWLEDGE IN THE AREA OF MEDICAL AND SURGERY
Journal of Medical Research and Surgery
PROVIDES A UNIQUE PLATFORM TO PUBLISH ORIGINAL RESEARCH AND REMODEL THE KNOWLEDGE IN THE AREA OF MEDICAL AND SURGERY
 Indexed Articles
Indexed ArticlesSelect your language of interest to view the total content in your interested language
Benslima Najwa1,2*, Kassimi Mariam1, Chikhaoui Ines3, Berrada Sophia1, Chikhaoui Nabil4, Mahi Mohamed1, Ahid Samir4,5
1Faculty of Medicine, Radiology, Mohammed VI University of Health Sciences (UM6SS), Casablanca, Morocco
2Methodological Support Unit, Mohammed VI University of Health Sciences (UM6SS), Casablanca, Morocco
3Faculty of Medicine, Dermatology, Mohammed VI University of Health Sciences (UM6SS), Casablanca, Morocco
4Faculty of Medicine, Emergency Department, Ibn Rochd Hospital, Hassan II University, Casablanca, Morocco
5Faculty of Pharmacy, Mohammed VI University of Health Sciences (UM6SS), Casablanca, Morocco
Correspondence to: Benslima Najwa, Faculty of Medicine, Radiology, Mohammed VI University of Health Sciences (UM6SS), Casablanca, Morocco
Received date: July 31, 2022; Accepted date: August 25, 2022; Published date: September 02, 2022
Citation: Benslima N, Kassimi M, Chikhaoui I, et al. Magnetic Resonance Imaging in Breast Cancer: A Moroccan Retrospective Study and Literature Review
Perspectives. J Med Res Surg. 2022; 3(5): 86-90. doi: 10.52916/jmrs224086
Copyright: ©2022 Benslima N, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted
use, distribution and reproduction in any medium, provided the original author and source are credited.
Objective: The aim of this work is to evaluate the benefit of Magnetic Resonance Imaging (MRI) to
detect breast cancer and to determine the operative management.
Methods: In this retrospective, single-center study of 68 patients with breast lesions and who were
consulted at the radiology Department of the Cheikh Khalifa University Hospital, in Casablanca,
from May 2015 to January 2021. They underwent initially mammography and ultrasonography and
secondary breast MRI. MRI studied the size, location, multifocality, multicentricity, bilaterality, contrast
enhancement characteristics, radiological, and pathological axillary involvement. Consistency between
MRI-BIRADS and MG+US-BIRADS, as well as the correlation with histological findings were also studied.
Results: The correlation between the BI-RADS categories of MRI and MG+USG was statistically significant
(p<0.01) as was between histopathological diagnosis and MRI BI-RADS. In the same way, MRI detects
more lesions than MG-US mainly to look for multifocality and multicentricity before surgical treatment
(p<0.01), 14.7% (n:10) was multicentric, and 13.2% (n:9) was ipsilateral. Preoperative breast MRI has
90% of sensitivity and 93% of specificity to detect malignant lesion versus (80%, 90%) with MG+US.
Conclusion: Breast MRI is an interesting and reliable tool for imaging breast neoplasms. It has to be
reserved as a problem-solving modality to be used in conjunction with conventional methods. However,
it is not denuded of disadvantages such as high cost and false-positive finding.
Breast cancer, MR mammography, Preoperative, Magnetic Resonance Imaging
Magnetic Resonance Imaging (MRI) is an important tool in breast imaging with multiple clinical indications. Since 25 years ago, breast MRI is approved by Food and Drug Administration (FDA) for detection of cancer especially in screening women with genetic high risks BRCA1 mutation (sensitivity >90% and variable specificity (range 30-90%) [1,2]. Previous researches [3-5], show that screening for women with extremely dense breasts using MRI is cost-effective, when applied at a 4-year interval.
Breast Imaging-Reporting and Data System (BI-RADS) MRI lexicon to standardise breast MRI reports worldwide is released in 2013 [6]. However, there is proof that MRI before breast conservation surgery, it is most sensitive to detect small malignant lesions [7]. However, there is no significat survival result for nonpalpable breast tumors [8,9]. Preoperative MRI is still beneficial to characterise the precise local extent and evaluation of surgical treatment response [2]. Some breast cancers can have multicentric or multifocal lesions in the ipsilateral breast, have long extension to pectoral muscle. For a better therapeutic management, the surgeon need to have an imaging check before breast conservation.
The usually preoperative imaging is mammography and breast ultrasonography. Actually preoperative breast MRI imaging can be included [10,11]. False-positive findings on breast MRI are common. Therefore, histologic confirmation of suspicious indeterminate MRI findings is necessary. This purpose will provide a comprehensive overview of the current clinical advantage of preoperative MRI in breast cancer in Morocco.
This is a retrospective single-center study, a descriptive analysis of 68 patients with breast disease who had a Mammography (MG), Ultrasonography (US), and MR imaging at the radiology Department of the Cheikh Khalifa University Hospital, in Casablanca, from May 2015 to January 2021. We included 68 female patients with dense breasts, malignant breast tumor detected on clinical examination, bloody nipple discharge, or patients who underwent preoperative MRI. We used the Breast Imaging Reporting and Data System (BI-RADS) classification to describe the overall breast constitution and only patients with type C (heterogeneously dense) and D were included (extremely dense). We excluded pregnant women and other patients with contraindication to MRI. The final diagnosis of malignant breast cancer was confirmed by percutaneous needle biopsy. The ethical comity of our hospital approved the study. The data collection was carried out anonymously by a computer system for patient data.
Statistical data analysis measurements were made by SPSS statistics for Windows (IBM SPSS Statistics for Windows, Version 26.0. Armonk, NY: IBM Corp), and using Khi-2 and T. Student tests. Specificity, sensitivity, and calculation and presentation of the ROC curve in accordance with BI-RADS classification. Differences were deemed to be statistically significant if the p-value is <0.05.
All patients underwent baseline ultrasonography and mammography.
A breast MRI was indicated for further therapeutic management. It was performed with a General Electric Signa HD (1.5 Tesla) superconductive magnetic system, using a bilateral, dedicated four channel phased array breast coil in the prone position. Standard imaging was performed with axial fast spin-echo (FSE) T1 and an axial and sagittal FSE T2, axial fat suppressed T2, axial diffusion, and fat suppressed dynamic enhanced T1 sequences.
We studied the size, location, number, multicentricity, bilaterality, radiological, and pathological axillary involvement. All examinations were interpreted by a senior radiologist (10 years of experience) and based on BI RADS classification.
We studied the consistency between MRI-BIRADS and MG+USBIRADS, as well as the correlation with histological findings, and the number of lesions detected by MG-US and MRI.
We studied 68 females patients, the mean patient age was 48.6 years +/- 11.5 (age range, 23-74 years). 5 patients (7%) had a personal carcinologic antecedent, and 25 patients (36.8%) had a familial one (Table 1).
N |
% |
|
| Age (years)* | 48 |
+/- 11.5* |
| Symptoms | ||
| Mastodinia | 25 |
(36.8) |
| Inflammatory symptoms | 3 |
-4.4 |
| Swelling | 2 |
-2.9 |
| Galactorragia | 5 |
-7.4 |
| Abcess | 2 |
-2.9 |
| Orange skin | 4 |
-5.9 |
| Mass | 61 |
-89.7 |
| Axillary node | 19 |
-27.9 |
| Menopause | 42 |
-61.8 |
| Diabetes | 9 |
-13.2 |
| Hypertension | 4 |
-5.9 |
| Obesity | 22 |
-32.4 |
| Familiar cance | 25 |
-36.8 |
| * Mean +/- SD | ||
58 (60.5%) patients had high breast density (type C and type D of BIRADS classification of breast density).
The MRI imaging was mainly indicated to study size, location, multi foci, multicentricity, bilaterality, inflammation breast, and parietal invasion (Table 2).
| Indication | MRI |
N (%) |
|
| Cancer primitif | 27 (39.7) |
| Multicentricity | 10 (14.7) |
| Multicentricity | 9 (13.2) |
| Pectoral infiltration | 8 (11.8) |
| Therapeutic evaluation | 3 (4.4) |
| Ductal ectasy | 3 (4.4) |
| Dystrophie fibrocyst | 1 (1.5) |
| Inflammation | 1 (1.5) |
| Metastasis lymphadenopathy | 1 (1.5) |
BI-RADS classification was used in mammo-ultrasonography and MRI, we classified BIRADS 4 (41.2%, n: 28) with MG+US, (versus 16.2%, n:11) with MRI, and most lesions classified already BIRADS 5 using (MRI 58.8%, n:40) versus (36.8%, n:25) using MG+US. The BI-RADS classification found in MG-US was upgraded in MRI (p<0.01). Five patients with high genetic risk, breast MRI detected infra centimetric lesions in 2 patients classified initially as BIRADS 4 (Figure 1).
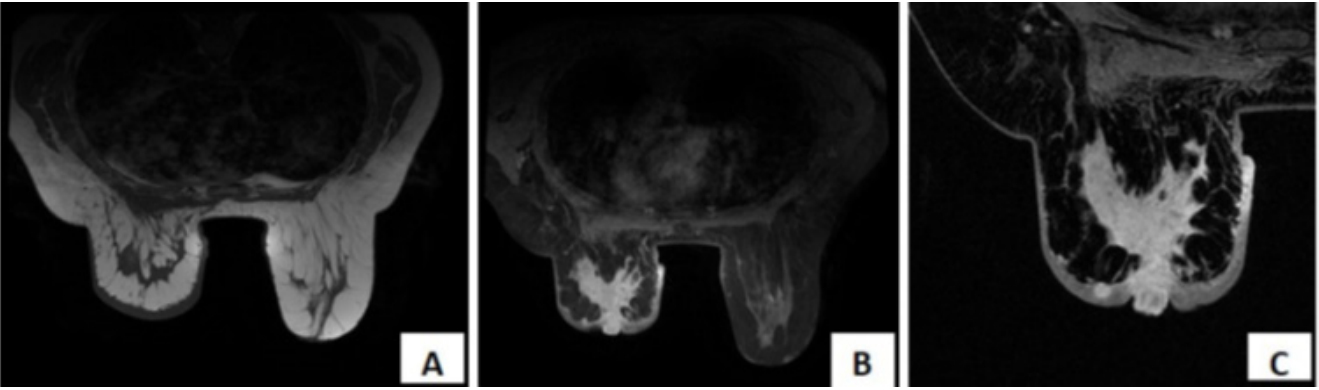 Figure 1: 30-years-old women with a long history of mastitis not improved
with usual traitement. Mammography and ultrasonography were difficult
to interpret because of their high density (Breast-Imaging-Reporting and
Data System 0). Axial plan of breast MRI in A): S T1; B): SP T2STIR; and C):
T1- weighted contrast-enhanced showed an irregular mass in the upper
outer quadrant and intensive enhancement. Microbiopsy confirmed
carcinomatoide mastitis.
Figure 1: 30-years-old women with a long history of mastitis not improved
with usual traitement. Mammography and ultrasonography were difficult
to interpret because of their high density (Breast-Imaging-Reporting and
Data System 0). Axial plan of breast MRI in A): S T1; B): SP T2STIR; and C):
T1- weighted contrast-enhanced showed an irregular mass in the upper
outer quadrant and intensive enhancement. Microbiopsy confirmed
carcinomatoide mastitis.More lesions were detected on MRI than MG-US (p<0.01). 14.7% (n:10) was multicentric, and 13.2% (n:9) was ipsilateral (Table 2, 3).
MG+US |
MRI |
|
N (%) |
N (%) |
|
| BI-RADS | ||
| 2 | 6 (8,8) |
7 (10.3) |
| 3 | 9 (13,2) |
8 (11.8) |
| 4 | 28 (41,2) |
11 (16.2) |
| 5 | 25 (36,8) |
40 (58.8) |
| 6 | 0 (0) |
0 (0) |
| Number of lesions | ||
| 1 | 91.2 (62) |
72.1 (49) |
| 2 | 7.4 (5) |
22.1 (15) |
| 3 | 1.5 (1) |
5.8 (4) |
MRI was indicated for nine patients (13.2%) to look for bilaterality. We confirmed malignancy for seven of them verified histologically. Multifocality and/or multicentricity were suspected in 14 patients (20.5%), among them, and eight of them underwent a non-conservative treatment. In only one case breast MRI objectified a multifocality non-diagnosed in conventional imaging.
MRI was performed in tree cases for patients follow-up and confirmed recurrences.
A breast MRI was indicated and allowed the diagnosis of carcinomatous mastitis in 2 patients with inflammatory breast unresolved after antibiotic therapy (Figure 2).
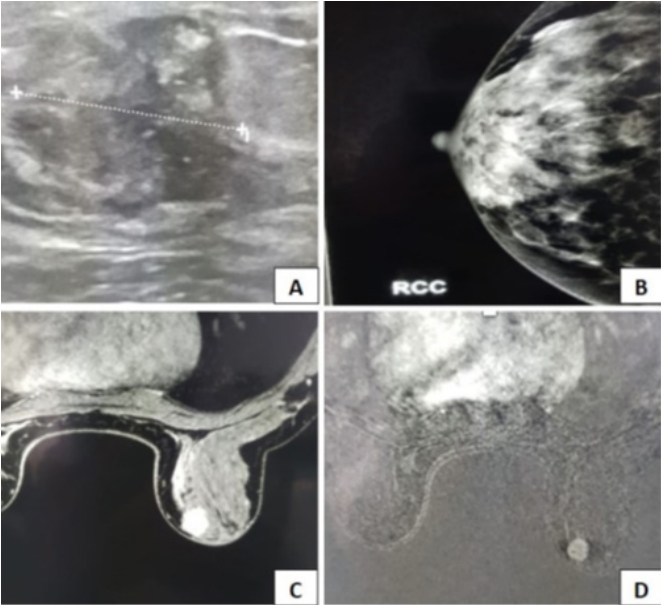 Figure 2: 330-years-old, women with high risk of familial breast cancer. Self
palpation indicate right breast masse with mastodynia; A,B): Mammography
exploration showed irrégular, heterogenious masse of inner upper quadrant
(BIRADS 4), sonography guided microbiospy conclued to an infiltrating
lobular carcinoma; C,D): Preoperative breast MRI imaging showed irregular,
spicular masse with heterogenously enhancing, without additional masse
contralateral.
Figure 2: 330-years-old, women with high risk of familial breast cancer. Self
palpation indicate right breast masse with mastodynia; A,B): Mammography
exploration showed irrégular, heterogenious masse of inner upper quadrant
(BIRADS 4), sonography guided microbiospy conclued to an infiltrating
lobular carcinoma; C,D): Preoperative breast MRI imaging showed irregular,
spicular masse with heterogenously enhancing, without additional masse
contralateral.All lesions were verified by micro-biopsy. All histopathological findings were reported in (Table 4).
| Histological types | N (%) |
| Benign | 19 (28) |
| Fibrocystic mastopathy | 10 (14.7) |
| Simple cyst | 3 (4.4) |
| Ductal inflammation | 2 (2.9) |
| Breast node | 1 (1.5) |
| Remodeled cyst | 1 (1.5) |
| Sclerosing adenosis | 1 (1.5) |
| Fibroadenoma | 1 (1.5) |
| Malignant | 48 (70.7) |
| Invasive ductal carcinoma | 28 (41.2) |
| Invasive lobular carcinoma | 11 (16.2) |
| In situ ductal carcinoma | 4 (5.9) |
| Indifferentied ductal carcinoma | 3 (4.4) |
| Lobular indifferentied carcinoma | 1 (1.5) |
| Papillary carcinoma | 1 (1.5) |
Eight patients (11.9%) had a mastectomy and 42 (62.7%) had breast conservation.
In our study, preoperative breast MRI has 90% of sensitivity and 93% of specificity to detect malignant lesion versus (80%, 90%) with MG + US (Figure 3).
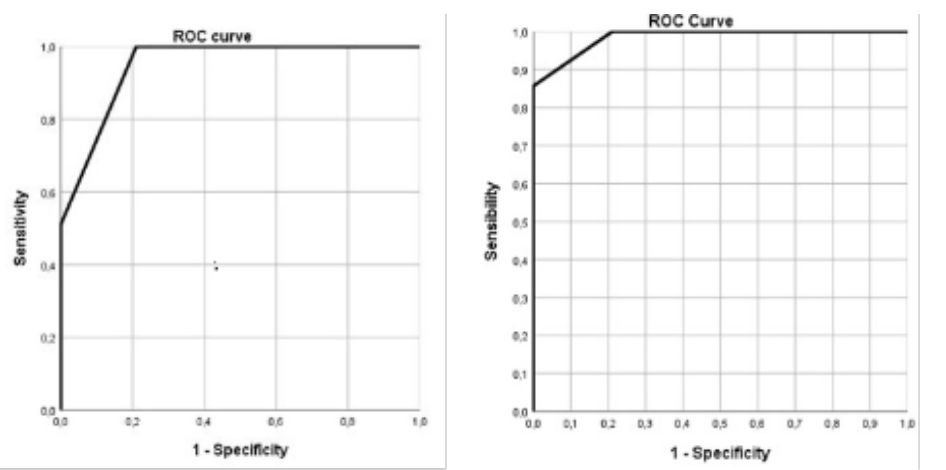 Figure 3: Roc curve for BIRADS classification result with echo-mammography
and breast MRI shows a): sensitivity; and b): sensibility.
Figure 3: Roc curve for BIRADS classification result with echo-mammography
and breast MRI shows a): sensitivity; and b): sensibility.Breast MRI is an emerging technic that revolutionizes the management of women with known or suspected breast cancer. To the best of our knowledge, it is the first study in Morocco to analyze the benefit of MR-mammography in the preoperative management of breast cancer.
MRI is a relevant tool in breast cancer imaging, and dynamic contrast-enhanced MRI is the keystone of any breast MRI protocol, as it provides excellent sensitivity and good specificity for breast cancer diagnosis [12].
It offers high-resolution morphological and functional parameters about angiogenesis as tumor-specific feature. The superiority of MRI is related to its high sensitivity in tumor detection because of the consistent contrast enhancement of breast cancer lesions.
Standard breast DCE-MRI protocols contain a three-plane localizer, a water-sensitive sequence (T2-weighted), T1- weighted unenhanced, and two or more T1-weighted contrastenhanced sequences. These Sequences are performed with or without fat saturation, and post processing is dedicated for subtraction and Maximum Intensity Projection (MIP) [13].
Different studies encourage the use of abbreviated MRI protocols that have shown diagnostic accuracy comparable to that of the conventional full MRI protocol [14,15].
One of the famous studies that investigate the use of an abbreviated breast MRI protocol was a prospective singlecenter study guided by Kuhl, et al. [16] in 2014 including unenhanced T1-weighted imaging without fat saturation, First contrast-enhanced T1-weighted imaging without fat saturation, subtraction, and MIP. In our study, we used standard breast MRI protocol since our technicians are familiar with it.
MRI defines tumor size, recognizes additional malignant lesions, and breasts with high density [17]. It seems to be particularly more contributive than mammography and ultrasound for evaluating invasive lobular cancer, ductal carcinoma in situ, multifocal/multicentric disease, and lesions with a presumed associated extensive intraductal component [18].
In our retrospective study, MRI was indicated mainly for suspected multifocal or multicentric disease and in dense breasts.
Previously published studies reported that MRI for breast cancer is highly sensitive (83%-100%) [19]. It supported the presumption that non-enhancing lesions were benign and did not require biopsy, but it shouldn’t be used to overrule or replace a biopsy. These findings are concordant with our study.
When breast cancer is detected or confirmed, MRI provides consistent staging of disease for treatment arranging [19]. Dynamic Contrast-Enhanced MRI (DCE-MRI) yields morphological and functional tumor characteristics, with excellent sensitivity and variable specificity [20]. To overcome limitations in specificity additional MRI parameters should be combined. Women with breast cancer who performed breast MRI in the preoperative evaluation were compared with the results for women who did not undergo breast MRI [21]. The rate of local tumor recurrence after treatment was significantly reduced among the patients who had undergone preoperative MRI [22]. MRI reduces positive resection margins in patients with conservative treatment. Recent observational study confirmed that positive margin resection is associated with high risk of local recurrence. Reoperations are associated with physical and emotional burden for patients, and higher healthcare costs [23]. Consequently, the re-excision rate is a national breast treatment quality indicator. In our study, preoperative breast MRI reduced mastectomies and no secondary surgery was necessary.
Ryu J, et al. [11] evaluated the effect of preoperative MRI on survival outcomes in patients with early breast cancer, and conclude that preoperative MRI did not affect survival outcomes in T1–2 breast cancer patients who received breast-conserving therapy. Recent study [24] carried out on young women (<35 years-old) with breast cancer detected on mammography, concluded that MRI detects more additional malignant lesions, makes it possible to reduce recurrences and surgical revisions. In young patients, breast MRI was associated with less primary mastectomies but with an increase in surgical margin involvement and an increase in secondary mastectomy rates [25]. Houssami, et al. evaluated the impact of contralateral breast cancer detection and reported a relative increase in survival due to its early detection [26].
Breast cancers were classified according to the Union for International Cancer Control (UICC) TNM classification 8th edition [27] to into Ductal Carcinoma In Situ (DCIS) and invasive cancers. Lobular Carcinoma In Situ (LCIS) was classified as a lesion not needing treatment, except pleomorphic LCIS, which was treated as DCIS. Lobbes, et al. [28] showed that preoperative breast MRI reduce mastectomies and positive surgical margins in invasive lobular cancer, but increase number of mastectomies in ductal cancers.
MRI is recommended for high-density breast tissue as proposed by many recent randomized studies [3]. Van Goethem, et al. [29] reviewed 67 patients with dense breasts and a malignant breast tumor intended for conservative surgery and concluded that MRI was more accurate in assessing tumor extent and multifocality in patients with dense breasts.
There were several limitations to our study including technical challenges related to the absence of a control group. We are looking to perform another larger prospective study and include a control group with only MG-US and another with MG-US + MRI to evaluate MRI value and enlarge indications.
Breast MRI is considered the most useful in patients with proven breast cancer to assess for multifocality/multicentricity disease, chemotherapy response, or tumor recurrence or to identify the primary site in patients with occult breast cancer. Its sensitivity is high but the specificity remains low responsible for false positives. Hence the interest in developing MRI-guided biopsies and scouting to reduce false positives. Further studies are recommended to enlarge the utility of breast MRI.
No.
The autors declare that they have no conflict of interests.
