 Journal of Medical Research and Surgery
PROVIDES A UNIQUE PLATFORM TO PUBLISH ORIGINAL RESEARCH AND REMODEL THE KNOWLEDGE IN THE AREA OF MEDICAL AND SURGERY
Journal of Medical Research and Surgery
PROVIDES A UNIQUE PLATFORM TO PUBLISH ORIGINAL RESEARCH AND REMODEL THE KNOWLEDGE IN THE AREA OF MEDICAL AND SURGERY
 Journal of Medical Research and Surgery
PROVIDES A UNIQUE PLATFORM TO PUBLISH ORIGINAL RESEARCH AND REMODEL THE KNOWLEDGE IN THE AREA OF MEDICAL AND SURGERY
Journal of Medical Research and Surgery
PROVIDES A UNIQUE PLATFORM TO PUBLISH ORIGINAL RESEARCH AND REMODEL THE KNOWLEDGE IN THE AREA OF MEDICAL AND SURGERY
 Indexed Articles
Indexed ArticlesSelect your language of interest to view the total content in your interested language
Ramsha Fatima Qureshi, Sadaf Nasir, Rabiya Siraj, Ayesha Shayan* , Uzma Panhwer
, Uzma Panhwer , Rabia Ahmed Siddiqui
, Rabia Ahmed Siddiqui
Department of Radiology, Liaquat National Hospital, Karachi, Pakistan.
Correspondence to: Ayesha Shayan, Department of Radiology, Liaquat National Hospital, Karachi, Pakistan.
Received date: January 24, 2025; Accepted date: February 24, 2025; Published date: March 03, 2025
Citation: Qureshi RF, Nasir S, Siraj R, et al. Magnetic Resonance Imaging (MRI) in Primary Amenorrhea: A Comprehensive Analysis J Med Res Surg. 2025;6(2):22-26. doi: 10.52916/jmrs254161
Copyright: ©2025 Qureshi RF, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Objective: This study aims to investigate the frequency and underlying causes of primary amenorrhea utilizing MRI as a diagnostic tool. Material and Methods: Cross sectional prospective study was conducted at Department of Radiology, Liaquat National Hospital, Karachi for 1.5 years. However, sample size was limited due to very low prevalence. The uterus was examined in terms of normal growth and developmental abnormalities, such as rudimentary uterus, agenesis and hypoplasia. The ovaries were evaluated in terms of normal development, location anomalies, agenesis, presence of ovotestis and hypoplasia. Patients with ovarian tissue showing normal, hypoplastic, unilateral agenesis or location anomalies were examined for Müllerian duct anomalies. The cause of primary amenorrhea was detected using pelvic MRI as per operational definition. Results: In our study, a total of 14 patients were included who presented with complaints of primary amenorrhea. Out of these, 5 were diagnosed on mri as gonadal dysgenesis and 7 were diagnosed with mullerian duct abnormalities. While 2 were diagnosed with male pseudohermaphroditism and imperforate hymen. Among those who were diagnosed with gonadal dysgenesis, about 4 had sawyer syndrome while about 1 had ovarian hypoplasia. Among patients who had mullerian duct abonrmalities, about 5 had Mayer-Rokitansky-Küster-Hauser (MRKH) syndrome which was the overall most common anomaly observed in our study. Conclusion: In conclusion, MRI is a useful modality that aids in early diagnosis of primary amenorrhea which helps in early intervention and surgical correction requiring multidisciplinary approach so as to aid in puberty, fertility and psychological care of the patient.
Magnetic Resonance Imaging (MRI), Primary amenorrhea, Mayer-Rokitansky-Küster-Hauser (MRKH) syndrome, Mullerian Duct Anomalies (MDAS)
Primary amenorrhea, defined as the non-initiation of menarche by 14 years in the absence of secondary sexual characteristics or the lack of menses by 16 years amidst normal growth and secondary sexual characteristics, poses a significant medical condition [1]. It stands as the sixth leading cause of female infertility, affecting 2–5% of women during their reproductive years and similarly impacting 2–5% of adolescent girls [2,3]. It's crucial to underscore that amenorrhea, while a symptom, is not a disease per se, and its origins can be traced from the hypothalamic-pituitary axis to the uterus-ovary. Ensuring normal menstruation necessitates the standard functioning of neuroendocrinological and embryological development, along with a consistent genetic makeup. The condition can notably impact the physical and psychological health of the affected individual [4].
While some factors contributing to this condition may be reversible through basic medical or surgical interventions, certain cases may present more complex challenges, rendering menstruation entirely unachievable [5]. The identification of the underlying cause is paramount to select an apt treatment modality. Various methodologies, attributable to the diverse etiology, are utilized to diagnose primary amenorrhea [6-7]. Both hormone and karyotype analyses play pivotal roles in pinpointing endocrine and cytogenetic abnormalities, respectively [8]. Radiological imaging methods are deployed to discern anatomical disorders, with Ultrasonography (US) commonly employed to visualize the female genital organ anatomy and anomalies, albeit with limitations such as gas artifacts restricting the Field of View (FOV) [9-10]. In scenarios necessitating advanced imaging, Magnetic Resonance Imaging (MRI) emerges as the preferred modality, offering enhanced soft tissue resolution, elimination of ionizing radiation, multiplanar imaging capability, and a non-invasive approach for detailed anatomical evaluations [11-12]. A study conducted by Gündoğdu et al, involving patients undergoing pelvic MRI for primary amenorrhea, identified Gonadal dysgenesis in 41.1% and Mullerian duct anomalies in 58.8% of the cases [13].
Primary amenorrhea, while a physical condition, also casts social and psychological ramifications, especially given its diagnosis typically during adolescence. It is imperative to navigate through this phase by identifying the most suitable approach [14,15]. In instances where primary amenorrhea is presented, the initial step post-elimination of pregnancy possibility involves determining the etiology. MRI has ascended as the imaging modality of choice for evaluating primary amenorrhea, especially when ultrasonography is limited. However, a notable gap exists in local data regarding prevalence and pattern. In conclusion, ensuring early diagnosis and intervention is vital to mitigate potential complications [16,17].
Primary Amenorrhea: Primary amenorrhea will be principally defined as an absence of menarche by 15 years of age irrespective of secondary sex characteristics or an absence of menarche by 13 years of age in patients without developing secondary sex characteristics.
Causes of Primary Amenorrhea: Patients undergoing MRI will be evaluated for any one of the following causes:
Cross sectional study and prospective.
Study will be conducted at Department of Radiology, Liaquat National Hospital, Karachi.
1.5 years.
The sample size was calculated through Sample Size Calculator by Wan Nor Arifin (Available at https://wnarifin.github.io/ssc/ss1prop.html) by taking prevalence of anatomic abnormalities=82.3% Ref, margin of error=9%.The total calculated sample size was 70 patients. However, sample size was limited due to very low prevalence.
Non-probability consecutive.
Patients with history of primary amenorrhea referred to the Department of Radiology, Liaquat National Hospital, Karachi meeting inclusion criteria will be enrolled in the study. After taking informed consent, pelvic MRI will be performed. The MRI examination will be undertaken using a 1.5 Tesla MRI device with six channel array coils, while the imaging protocol for the pelvic MRI comprised T1-weighted, T2-weighted, and T1- and T2-weighted fat suppressed sequences in the axial plane and T2-weighted sequences in the coronal and sagittal plane. The pelvic examination will include the evaluation of the presence and morphology of the uterus, ovaries and vagina. The uterus will be examined in terms of normal growth and developmental abnormalities, such as rudimentary uterus, agenesis and hypoplasia. The ovaries will be evaluated in terms of normal development, location anomalies, agenesis, presence of ovotestis and hypoplasia. Patients with ovarian tissue showing normal, hypoplastic, unilateral agenesis or location anomalies will be examined for Müllerian Duct Anomalies (MDAs). The cause of primary amenorrhea will be detected using pelvic MRI as per operational definition. The findings of quantitative variables and qualitative variable will be entered in proforma attached as annexure.
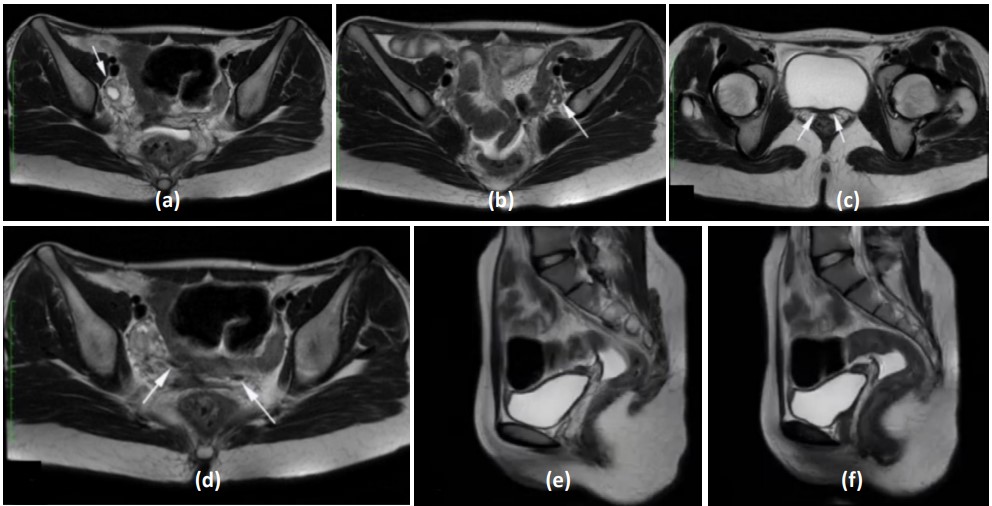 Figure 1: Case 1: MRKH syndrome. Axial T2-WI. (a) and (b): Shows normal ovaries while; (c) and (d): Shows rudimentary horn (marked by arrows). Sagittal T2-WI, (e) and (f): Demonstrate a triangular shape between bladder and rectum, which is the fibro-adipose remnant tissue of the aplastic uterus.
Figure 1: Case 1: MRKH syndrome. Axial T2-WI. (a) and (b): Shows normal ovaries while; (c) and (d): Shows rudimentary horn (marked by arrows). Sagittal T2-WI, (e) and (f): Demonstrate a triangular shape between bladder and rectum, which is the fibro-adipose remnant tissue of the aplastic uterus.
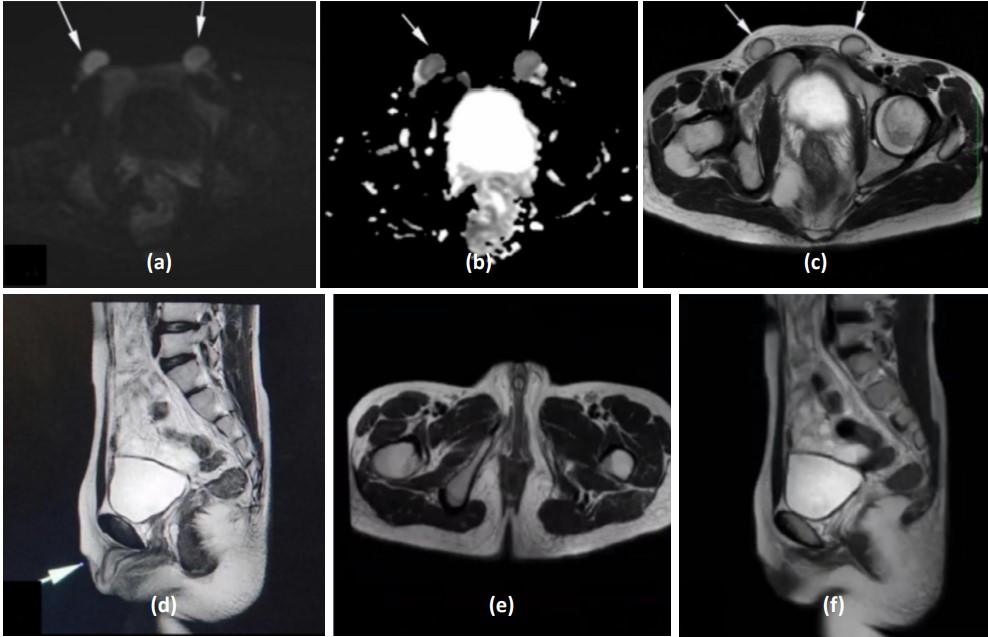 Figure 2: Case 2: Male pseudo hermaphroditism. (a), (b) and (c): DWI, ADC and Axial T2-WI. Shows two well-defined ovoid areas with T2 intermediate signals, hypointense rim and restricted diffusion in bilateral inguinal canals representing undescended testes. (d): Sagittal and Axial T2-WI; (e): Show absent corpus spongiosum, however differentiated corpora cavernosa are seen extending upto and projecting between labia majora in the form of enlarged clitoris. (f): Sagittal T2-WI. Demonstrate non visualization of uterus, ovaries and cervical canal.
Figure 2: Case 2: Male pseudo hermaphroditism. (a), (b) and (c): DWI, ADC and Axial T2-WI. Shows two well-defined ovoid areas with T2 intermediate signals, hypointense rim and restricted diffusion in bilateral inguinal canals representing undescended testes. (d): Sagittal and Axial T2-WI; (e): Show absent corpus spongiosum, however differentiated corpora cavernosa are seen extending upto and projecting between labia majora in the form of enlarged clitoris. (f): Sagittal T2-WI. Demonstrate non visualization of uterus, ovaries and cervical canal.Magnetic Resonance Imaging (MRI) plays a crucial role in the diagnosis and management of primary amenorrhea, particularly in cases where there are suspicions of anatomical abnormalities like mullerian anomalies. Several studies emphasize the significance of MRI in accurately diagnosing conditions such as Mayer–Rokitansky–Küster–Hauser syndrome (MRKH) and other causes of primary amenorrhea. There are several potential causes of primary amenorrhea, which can be broadly categorized as describe in table 1.
The two conditions that are most prevalent worldwide include Mullerian Duct Anomalies (MDAS) and gonadal dysgenesis. MDAS is predominantly found in population of Asia and Africa, whereas gonadal dysgenesis is prevalent in the western population. In this study also, mullerian duct anomalies were the most common etiology reported in 50 % of cases and gonadal dysgenesis was 35.7 %.
The two müllerian ducts are embryonic structures which develop into the female reproductive organs i fallopian tube, uterus, cervix and upper vagina. In the normal process of development the mullerian ducts join together along the body midline in order to create these structures. Mullerian Duct Anomalies (MDAS) occurs when there is an abnormality in the outgrowth of these ducts. These anomalies can be classified into several categories based on the stage of development that was affected.
The first step in investigating primary amenorrhea is taking a detailed history and performing a physical examination of the patient. But newer studies show types of MRKH syndrome patients with normal puberty development but primary amenorrhea figure 1, whereas complete androgen insensitivity syndrome requires that all patients develop externally normal breasts but have scanty body hair.
Among other tools for diagnosis include biochemical tests for LH, FSH, estradiol, testosterone and other hormones as well as karyotype and imaging technique. Pelvic ultrasound scanning is used in the evaluation of these anatomical causes while MRI is done when the uterus is not visualized on ultrasound.
Magnetic Resonance Imaging (MRI) is critical in the evaluation of patients with primary amenorrhea especially when there is a suspicion of anatomical defects such as mullerian anomalies and after extensive secondary amenorrhea workup. Many other studies have found MRI to be useful in the proper diagnosis of primary amenorrhea such as Mayer-Rokitansky Küster–Hauser syndrome (MRKH).
The accuracy of diagnosis: MRI complements the findings made in hysteroscopy by ruling out anomalous uterine structures and defects including absent uterus and delineation of the normal structural diseases that cause primary amenorrhea.
A dedicated MRI protocol with a focus on high-resolution, multiplanar T2-weighted sequences oriented along the long axis of the uterus is considered the best approach for comprehensive evaluation and accurate diagnosis of uterine congenital abnormalities Surgical planning: MRI provides detailed imaging of mullerian structures, ovaries, vagina, and kidneys, which is essential for surgical planning in cases like MRKH syndrome. Comprehensive evaluation: combining clinical history, physical examination, biochemical evaluation, and MRI assessment by experienced radiologists is crucial for a well- established diagnosis in primary amenorrhea cases with an apparently absent uterus.
In conclusion, MRI is a useful modality that aids in early diagnosis of primary amenorrhea which helps in early intervention and surgical correction. The early diagnosis of these conditions is important and requires multidisciplinary approach so as to aid in puberty, fertility and psychological care of the patient.
The authors declare no conflict of interest.
