 Journal of Medical Research and Surgery
PROVIDES A UNIQUE PLATFORM TO PUBLISH ORIGINAL RESEARCH AND REMODEL THE KNOWLEDGE IN THE AREA OF MEDICAL AND SURGERY
Journal of Medical Research and Surgery
PROVIDES A UNIQUE PLATFORM TO PUBLISH ORIGINAL RESEARCH AND REMODEL THE KNOWLEDGE IN THE AREA OF MEDICAL AND SURGERY
 Journal of Medical Research and Surgery
PROVIDES A UNIQUE PLATFORM TO PUBLISH ORIGINAL RESEARCH AND REMODEL THE KNOWLEDGE IN THE AREA OF MEDICAL AND SURGERY
Journal of Medical Research and Surgery
PROVIDES A UNIQUE PLATFORM TO PUBLISH ORIGINAL RESEARCH AND REMODEL THE KNOWLEDGE IN THE AREA OF MEDICAL AND SURGERY
 Indexed Articles
Indexed ArticlesSelect your language of interest to view the total content in your interested language
Thaer M. Farhan1*, Huda Rashid Kamoona2
1.Associate Professor of Clinical Anatomy and Embryology, Department of Human Anatomy, College of Medicine, Al-Nahrain University, Baghdad,
Iraq
2.Assistant Professor of Human Anatomy, Department of Human Anatomy, College of Medicine, Al-Nahrain University, Baghdad, Iraq
Correspondence to: Thaer M. Farhan, Associate Professor of Clinical Anatomy and Embryology, Department of Human Anatomy, College of Medicine, Al-Nahrain
University, Baghdad, Iraq
Received date: January 16, 2021; Accepted date: January 29, 2021; Published date: February 5, 2021
Citation: Farhan TM, Kamoona HR (2021) MRI-Evaluation of Suprascapular Notch Morphometry and Its Clinical Applications. J Med Res Surg 2(1): pp. 1-6.
doi: 10.52916/jmrs214036
Copyright: ©2021 Farhan TM, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits
unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
The suprascapular notch, a depression on the lateral part of the superior border of the scapula, medial to the coracoid process, is covered by the superior transverse scapular ligament, which is converted into a foramen. Sometimes it might be ossified forming a complete osseous foramen. The Suprascapular Notch (SN) served as a passage for the Suprascapular Nerve (SSN). Study the morphology of the suprascapular notch and the suprascapular transverse ligament based on MRI, variations in shape and dimensions of the suprascapular notch. A group of 100 patients underwent MRI examination of the scapular region through the period from 10th July 2019 to 15th Feb 2020. Different morphological types of the suprascapular notch were encountered in the study, the most common type was type III, while type I was less common in the study. The symmetry of the morphological feature of SN bilaterally was seen in 51% of the cases. Conclusively, the symmetry of the suprascapular notch is not a constant feature bilaterally.
Suprascapular notch, Suprascapular nerve, Scapula, Shoulder pain, Shoulder MRI, Suprascapular nerve entrapment
The suprascapular notch, a depression on the lateral part of the superior border of the scapula, medial to the coracoid process, is covered by the superior transverse scapular ligament, which is converted into a foramen. Sometimes it might be ossified forming a complete osseous foramen. The Suprascapular Notch (SN) serves as a passage for the Suprascapular Nerve (SSN) [1- 3].The Superior Transverse Scapular Ligament (STSL) forms the roof of the suprascapular notch, which is the most common location of entrapment of the suprascapular nerve, a cause of shoulder pain and weakness [3,4] (Figure 1). The first description of suprascapular nerve entrapment syndrome at the site of the suprascapular notch was made by Kopell and Thompson [5,6]. The shape and size of the Suprascapular Notch (SN) are one of the most important risk factors in suprascapular nerve entrapment [7,8].
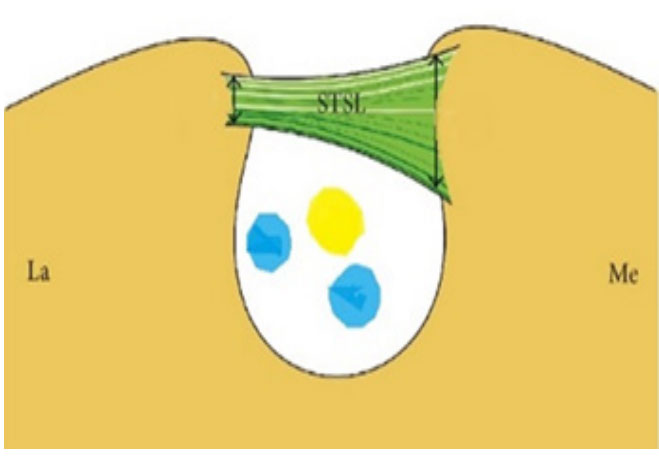 Figure 1: Suprascapular notch closed by suprascapular ligament, the
suprascapular nerve and veins pass below the ligament.
Figure 1: Suprascapular notch closed by suprascapular ligament, the
suprascapular nerve and veins pass below the ligament.The Superior Transverse Scapular Ligament (STSL) is a fibrous band connecting two borders of Suprascapular Notch (SN) on the upper border of the scapula. The Suprascapular Nerve (SSN) passes below the ligament through the opening while the suprascapular artery crosses over the ligament [2,9,10]. Evaluation of the morphology of the suprascapular notch region is important from a clinical point of view because it is the most common site of suprascapular nerve compression and injury. The suprascapular notch is characterized by variable morphology. However, its development is not well studied [11,12].
Anatomical variations and the anomalous or ossified superior transverse scapular ligament are also considered to be risk factors for suprascapular neuropathy [13]. The shape and morphology of the suprascapular notch is the most critical point that affects the etiology of nerve neuropathy like neuropraxia, for instance. the suprascapular notch was classified according to a fivefold classification (Type I, deeper than wider; Type II, equally deep and wide; type III, wider than deeper; type IV, bony foramen; type V, discreet notch [14,15].
A group of 100 patients underwent MRI examination of the scapular region through the period from 10th July 2019 to 15th February 2020. These 100 clinical cases were referred to the radiology department due to different medical complaints. The study is a retrospective type including already performed MRI examination of the shoulder region which renders the suprascapular region more feasible to be visualized and evaluated.
The inclusion criteria were as follows: both scapulae encompassed in a field of view; no artifacts; no pathologies concerning the scapulae. Based on visual assessment and measurements. No fractures or direct trauma of the scapula. Measurements of the suprascapular notch and superior transverse scapular bar were taken with the help of digital scales and radiographic markers that are built in the MRI software system. The following suprascapular notch dimensions were measured: maximal depth, superior transverse diameter and middle transverse diameter were recorded. The data was analyzed statistically.
According to the above-mentioned dimensions, the SN is categorized into the following types based on their morphology and measurements:
Type I: MD dimension is longer than STD (Deeper notch)
Type II: MD and STD are equal
Type III: STD is longer than MD (Wider notch)
Type IV: Osseous foramen by a bony bridge
Type V: Discrete (Shallow) notch, Figure 2 (Illustration of SN types)
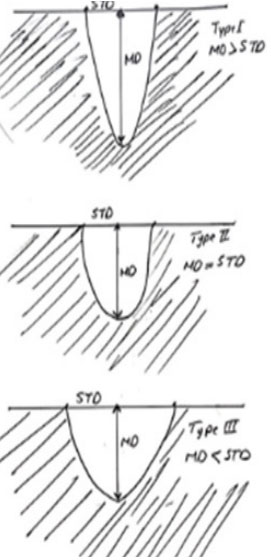 Figure 2: Types of the SN; Suprascapular Notch (SN), A: Shows type I; B:
Shows type II; C: Shows type III.
Figure 2: Types of the SN; Suprascapular Notch (SN), A: Shows type I; B:
Shows type II; C: Shows type III.The current study is characterized by simple and informative data that can be interpreted radiologically and anatomically. These data can be explained simply as follows: The total number of the examined patients by MRI technique was 100 patients, a total number of 200 scapular bones were studied by MRI bilaterally and retrospectively then were analyzed to classify suprascapular notches into five types. The following important data were recognized from the study
Regarding the morphology of the suprascapular notch; SN, the following percentage of occurrence were encountered in the study:
Type I: MD dimension is longer than STD, seen in 48 out of 200 scapulae (Figure 4).
Type II: MD and STD are equal, seen in 4 out of 200 scapulae (Figure 5).
Type III: STD is longer than MD, seen in 112 out of 200 scapulae (Figure 6).
Type IV: Osseous foramen by a bony bridge, seen in 10 out of 200 scapulae.
Type V: Discrete (Shallow) notch, seen in 26 out of 200 scapulae (Figure 7).
Table (1) for more explanations:
| SN type | No. of cases /200 scapulae | Percentage % from (200)scapulae | No. of cases have symmetry bilaterally per 100 patients | Percentage % of symmetry cases (51) |
|---|---|---|---|---|
| Type I | 48/ 200 | 24% | 8/ 100 | 17% |
| Type II | 4/ 200 | 2% | 1/ 100 | 2% |
| Type III | 112/ 200 ; | 56% | 33/ 100 | 64% |
| Type IV | 10/ 200 | 5% | 2/ 100 | 2% |
| Type V | 26/ 200 | 13% | 7/ 100 | 15% |
| Total | 200/200 | 100% | 51/100 | 100% |
Regarding the superior transverse scapular ligament and categorization according to its structure. In the current study, the best way to visualize the superior transverse scapular ligament, STSL; by using the MRI imaging technique with sagittal plane T1-weighted sequence, the STSL was found to be either
Table 2 for Superior Transverse Scapular Ligament (STSL), categorization according to its type and its frequency
| STSL type | No. of cases | Percentage % |
|---|---|---|
| Fibrous band | 180 | 0.9 |
| Ossified band | 12 | 0.06 |
| Non-visualized (absent) | 8 | 0.04 |
| Total | 200 | 1 |
The shoulder as well the scapular regions pain and dyskinesia is one of the common rheumatological complaints when its etiology is not yet fully described and understood; thus, many clinical studies were carried on to elaborate on this problem [16].
The most evident outcome from the current research was the symmetry of the suprascapular notches bilaterally. According to the study analysis, the SN symmetry is not a constant feature to be considered although, only a little more than half of the cases encountered were found to have the same features bilaterally [3].
According to Dunkelgrun et al, the shape and size of the SN are the most crucial factor in the etiology of the suprascapular nerve entrapment [17]. It could be supposed that humans with longer scapulae have deeper and narrow notches that may predispose to suprascapular nerve irritation and neuropathy. It may be also suggested that scapulae with a wider superior border have a shallower suprascapular notch [3,18,19].
The suprascapular nerve is one of the important structures that might be jeopardized and compressed either by muscular action or vascular effects of the nearby vessels or even a narrow suprascapular notch. The anatomical variations in the shape of the suprascapular notch, and its transformation into a foramen by complete or partial ossification of the superior transverse scapular ligament, are well-known reasons of suprascapular nerve entrapment. [20,21].
The suprascapular nerve may be compressed anywhere along its course to the site of innervation, most commonly at SN, the variations in morphometric dimensions of the notch, play a crucial role in suprascapular nerve entrapment [22].
Suprascapular nerve pathology is a rare diagnosis that is increasingly gaining popularity among the conditions that cause shoulder pain and dysfunction. The suprascapular notch is the common site for the entrapment of the suprascapular nerve. Suprascapular nerve compression usually presents with vague pain across the scapula or dull shoulder ache [23,24].
Several other anatomical variations in the region of suprascapular notch like thickened or multiband or even ossified suprascapular ligament should be taken in consideration when elaborate on the causes of suprascapular nerve entrapment [25]. In the cases where the suprascapular ligament is thick or even more evident, we can hypothesize that hypertrophy of the transverse scapular ligament creates a venous obstruction resulting in varicosities of the suprascapular vein which runs with the nerve under the ligament and causes a suprascapular neuropathy. As the suprascapular artery is the most easily recognized structure in the area, it may serve as a useful landmark of the suprascapular notch [8,26]. One of the limitations of the current study that the data were collected retrospectively
Different morphological patterns of the suprascapular notches have been encountered in the study, the most common type was type III when the STD is larger than MD (Wider notch). The symmetry of the suprascapular notch is not a constant feature bilaterally. The data suggest that the entrapment syndrome is more likely to be associated with a Type I notch because of its specific features.
The STSL can be visualized on the majority of shoulder MRIs and is best seen on sagittal T1-weighted images on our imaging protocol. Evaluation of the STSL can potentially help in identifying pathologic conditions affecting the suprascapular nerve.
We, the authors, greatly thankful for those workers at the Department of Radiology, Al-Imamain Teaching Hospital. It would not have been possible without the exceptional support of them.
The authors declare that there is no conflict of interest in the current work.
