 Journal of Medical Research and Surgery
PROVIDES A UNIQUE PLATFORM TO PUBLISH ORIGINAL RESEARCH AND REMODEL THE KNOWLEDGE IN THE AREA OF MEDICAL AND SURGERY
Journal of Medical Research and Surgery
PROVIDES A UNIQUE PLATFORM TO PUBLISH ORIGINAL RESEARCH AND REMODEL THE KNOWLEDGE IN THE AREA OF MEDICAL AND SURGERY
 Journal of Medical Research and Surgery
PROVIDES A UNIQUE PLATFORM TO PUBLISH ORIGINAL RESEARCH AND REMODEL THE KNOWLEDGE IN THE AREA OF MEDICAL AND SURGERY
Journal of Medical Research and Surgery
PROVIDES A UNIQUE PLATFORM TO PUBLISH ORIGINAL RESEARCH AND REMODEL THE KNOWLEDGE IN THE AREA OF MEDICAL AND SURGERY
 Indexed Articles
Indexed ArticlesSelect your language of interest to view the total content in your interested language
Gabriela Antúnez Lay1* , Juan Canales Pablo1
, Juan Canales Pablo1 , Tomas Merino Lara1
, Tomas Merino Lara1 , Wilmer Useche1, Diego Bazaes Núñez2
, Wilmer Useche1, Diego Bazaes Núñez2 , Paula Reyes Ortega1
, Paula Reyes Ortega1
1Departamento de Hemato-oncología, Facultad de Medicina, Pontificia Universidad Católica de Chile, Santiago de Chile.
2Departamento de Radiología, Facultad de Medicina, Pontificia Universidad Católica de Chile, Santiago de Chile.
Correspondence to: Gabriela Antúnez Lay, Departamento de Hemato-oncología, Facultad de Medicina, Pontificia Universidad Católica de Chile, Santiago de Chile.
Received date: May 28, 2024; Accepted date: June 17, 2024; Published date: June 24, 2024
Citation: Lay GA, Pablo JC, Lara TM, et al. Local Recurrence of Postoperative Prostate Cancer, Treatment and Toxicity with Stereotactic Body Radiotherapy (SBRT): A Case Report . J Med Res Surg. 2024;5(3):74-76. doi: 10.52916/jmrs244140
Copyright: ©2024 Lay GA, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted
use, distribution and reproduction in any medium, provided the original author and source are credited.
Background: Prostate cancer remains a major health concern worldwide, and postoperative recurrences are a significant challenge in its treatment. Various treatment modalities have been studied, but consensus on optimal strategies has not yet been established. This case report examines the feasibility and toxicity of stereotactic body radiation therapy (SBRT) as a therapeutic option for postoperative recurrences of prostate cancer. Case presentation: A 68-year-old man with a history of prostate cancer, initially treated with radical prostatectomy, who presented biochemical recurrence. Diagnostic imaging revealed a 9 mm nodule in the prostate bed, which was treated by SBRT guided by ultrasound visualization. The patient tolerated the treatment well, experiencing minimal genitourinary and gastrointestinal discomfort. Discussion: Multiple treatment alternatives exist for post-prostatectomy recurrence. Retrospective studies have suggested the efficacy of SBRT, although they lack robust empirical evidence. Recent investigations have highlighted the safety profile of SBRT, emphasizing the need for further exploration, particularly in image-guided radiotherapy. Conclusion: SBRT guided by ultrasound visualization emerges as a promising option for ablative treatment of postprostatectomy recurrence, offering a favorable safety profile and encouraging oncologic outcomes. Further research is needed to further clarify its role in salvage radiotherapy for localized recurrences.
Prostate cancer recurrence, Radiosurgery, Stereotactic Body Radiation Therapy (SBRT), Post-prostatectomy recurrence, Magnetic Resonance Imaging (MRI), Image-guided radiotherapy.
Prostate cancer is a prevalent disease worldwide, accounting for 7.1% of male malignancies in 2018 and 3.8% of cancer deaths [1]. In Chile, it is the most common oncologic disease in men, with an incidence of 61.3 per 100,000 inhabitants and the second leading cause of oncologic death [2]. Among the alternatives for curative treatment of the disease we can consider Radical Prostatectomy (RP), which is performed in one third of patients in the initial phase. After RP, recurrences are reported in 20-50% of cases, mostly biochemical, although there are cases in which macroscopic disease is observed in the prostatic bed and lymph node or distant metastases. The most frequent site of macroscopic recurrence is the prostate bed, this is known as Local Recurrence (LR). The finding of LR after RP has increased thanks to the use of new imaging techniques such as Positron Emission Tomography (PET) with choline or PSMA and Magnetic Resonance Imaging (MRI) [3].
The treatment of biochemical recurrence is well established in different international guidelines, however, there is no consensus on the optimal treatment for post-surgical local recurrences [4], these include surgery, cryoablation, external beam radiotherapy, brachytherapy and Stereotactic Body Radiotherapy (SBRT) [5]. This article addresses SBRT as a therapeutic alternative in postoperative prostate cancer LR, exploring its efficacy and toxicity through a case report.
This case is about a 68-year-old male patient with a previous history of prostate cancer in 2016 who was treated with radical prostatectomy and pelvic lymphadenectomy. Surgical biopsy reports adenocarcinoma in the right apex, Gleason 7 (4+3), which was resected with positive surgical border of 5 mm extension, without extra-prostatic involvement. Lymphadenectomy showed 6 lymph nodes resected to the right, without tumor and 2 resected to the left, without tumor. Prostate Specific Antigen (PSA) 6 weeks after surgery was <0.05 ng/ml. Patient had no follow-up until 2023 with PSA up to 2.89 ng/dL. An imaging study was requested with PET PSMA showing a 9 mm nodule in the prostate bed, in the posterior wall of the bladder over the Vesico-Urethral Anastomosis (VUA), with metabolic activity (SUVmax 2.5 g/ml), suggestive of LR (Figure 1).
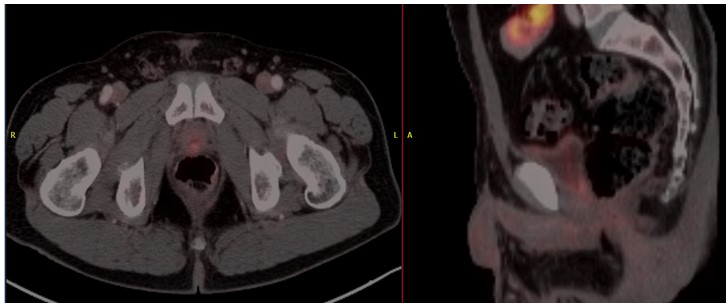 Figure 1: Axial (left) and sagittal (right) views from a diagnostic PET PSMA scan showing a 9 mm nodule in the prostate bed with metabolic activity, indicating Local Recurrence (LR).
Figure 1: Axial (left) and sagittal (right) views from a diagnostic PET PSMA scan showing a 9 mm nodule in the prostate bed with metabolic activity, indicating Local Recurrence (LR).The patient at the time of evaluation was in good general condition, without significant urinary symptoms (International Prostate Symptoms Score (IPSS)=2, due to nicturia), without incontinence, maintaining sexual activity without conflict.
Androgen Deprivation Treatment (ADT) was started and the patient proceeded to simulation according to protocol of rectal and bladder preparation with CT of the pelvis with contrast under ultrasound visualization (Clarity System®) for treatment planning of Stereotactic Body Radiation Therapy (SBRT) to the nodule in the prostate bed with 35 Gy in 5 fractions, weekly frequency (Figure 2).
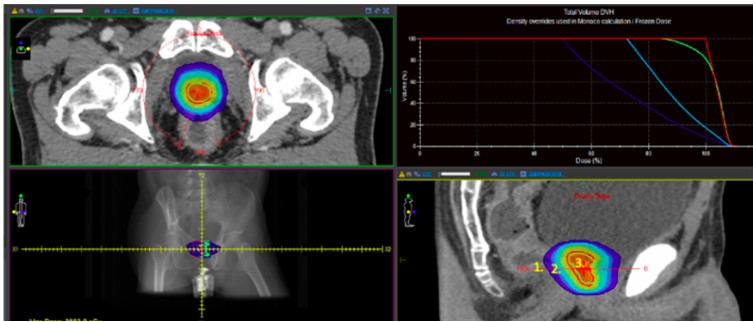 Figure 2: PTV_3500 (green). 1. Isodose 50% (blue). 2. Isodose 75% (light blue). 3. Isodose 100% (red).
Figure 2: PTV_3500 (green). 1. Isodose 50% (blue). 2. Isodose 75% (light blue). 3. Isodose 100% (red).|
Structure |
Dosimetric Criteria |
Value |
|
PTV_3500 |
V3325cGy ≥ 99% |
91.30% |
|
Bladder |
V3700cGy<10cm³ |
0.528cm³ |
|
|
V3500cGy<5cm³ |
1.556cm³ |
|
|
V1810cGy<40% |
3.84% |
|
Rectum |
V3500cGy<1cm³ |
0.255cm³ |
|
|
V2900cGy<10% |
2.16% |
|
|
V1810cGy<30% |
9.66% |
|
Penile Bulb |
V2950cGy<50% |
0% |
|
Right Femoral Head |
V1450cGy<5% |
0% |
|
Left Femoral Head |
V1450cGy<5% |
0% |
|
Urethra |
Dmax<3250cGy |
3260.3cGy |
The summary of the dosimetric parameters are in Table 1. The patient received treatment without incident. The maximum displacement was set as 2 mm in any direction on Clarity system. The average target movement was 1.03, 0.56 and 0.47 mm antero-superior, lateral and supero-inferior, respectively. Actual threshold was not exceeded in any fraction. Treatment was well tolerated with usual Genitourinary (GU) toxicity grade 1 (urgency) and IPSS=9 at the end of treatment. Gastrointestinal acute (GI) toxicity was grade 1 (proctalgia). At one month after the end of treatment the patient had few GU symptoms (IPSS=4) and resolution of proctalgia. Four months post radiotherapy the patient was asymptomatic from the GU and GI point of view with a IPSS=2. Regarding the biochemical control of the disease, the patient presents a decrease in PSA at six months (PSA of 0.02 ng/ml).
LR is an increasingly common clinical situation due to the increase in the availability and use of PSMA PET and/or MRI. The most common site of LR is in relation to the VUA, occurring in more than 66% of cases according to several series [7], which agrees with the presentation of the exposed patient.
There is currently no general consensus on the most appropriate treatment for RL in patients undergoing radical prostatectomy with a wide range of therapeutic possibilities. The local treatment of recurrence not only improves oncologic outcomes, but also makes it possible to delay additional treatments, such as ADT or chemotherapy, along with its burden of toxicity. One of the challenges associated with postprostatectomy ablation lies in achieving effective treatment while avoiding damage to surrounding structures, especially the rectum.
Some retrospective studies have assessed the use of SBRT for the treatment of LR, however, to date, there are no prospective studies validating its efficacy. Archer et al [8] published the results of the largest series evaluating SBRT in LR post RP. With a total of 117 patients they reported good local control with disease-free survival of 74% at 1 year, overall survival of 85% at 5 years and an acceptable GU and late GI toxicity profile of 25% at 1 year and 34% at 2 and 3 years.
Recently, Majewski et al [9] reported the safety profile of SBRT to local recurrence post prostatectomy and salvage external beam radiotherapy. No patients experienced grade 3 or greater acute toxicity, and 19% experienced grade 2 or less acute GU and/or GI toxicity.
The case presented did not experience acute toxicity of clinical significance, which is consistent with the results of the series noted above. This may be related to the lower volume of rectal and bladder irradiation, good performance of the patient prior to starting SBRT and use of radiotherapy guided by ultrasound visualization.
The use of image-guided radiation therapy in the context of LR has not been fully clarified. Michalet et al [10] presented preliminary results of a prospective registry with MR-guided SBRT of isolated postprostatectomy recurrence with good safety profile and excellent dosimetric results. There are no reports to date of local salvage treatment with ultrasound-guided radiotherapy (Clarity System®).
The use of SBRT in LR appears to be safe with a low proportion of patients with GU and/or GI toxicity. Several techniques are available to improve the accuracy of SBRT, including the use of ultrasound-guided treatments.
In conclusion, SBRT guided by ultrasound images (Clarity System®) is an alternative management in ablative treatment of post-prostatectomy local recurrence with a good safety profile and encouraging oncological results.
None.
