 Journal of Medical Research and Surgery
PROVIDES A UNIQUE PLATFORM TO PUBLISH ORIGINAL RESEARCH AND REMODEL THE KNOWLEDGE IN THE AREA OF MEDICAL AND SURGERY
Journal of Medical Research and Surgery
PROVIDES A UNIQUE PLATFORM TO PUBLISH ORIGINAL RESEARCH AND REMODEL THE KNOWLEDGE IN THE AREA OF MEDICAL AND SURGERY
 Journal of Medical Research and Surgery
PROVIDES A UNIQUE PLATFORM TO PUBLISH ORIGINAL RESEARCH AND REMODEL THE KNOWLEDGE IN THE AREA OF MEDICAL AND SURGERY
Journal of Medical Research and Surgery
PROVIDES A UNIQUE PLATFORM TO PUBLISH ORIGINAL RESEARCH AND REMODEL THE KNOWLEDGE IN THE AREA OF MEDICAL AND SURGERY
 Indexed Articles
Indexed ArticlesSelect your language of interest to view the total content in your interested language
Francisco J. Buils Vilalta1,2*, Juan José Sánchez Cano1,Joan Domènech1,2, Rosa Prieto Butillé1,2, Elisabet Homs Ferré1, Elia Bartra Balcells1, Pilar Martínez López1, Carla Morales Tugues1, Mariale García Durán1, Daniel del Castillo Déjardin1,2
1Deptartment of General and Digestive Surgery, Sant Joan University Hospital, Reus, Tarragona, Spain
2Rovira I Virgili University, Faculty of Medicine and Health Sciences, Surgery Unit, Tarragona, Spain
Correspondence to: Francisco J. Buils Vilalta, Deptartment of General and Digestive Surgery. Sant Joan University Hospital, Reus, Tarragona, Spain; E-mail:clinicsurg@gmail.com
Received date: April 15, 2020; Accepted date: April 26, 2020; Published date: May 02, 2020
Citation: Buils Vilalta FJ, Sánchez Cano JJ, Calvet JD, et al. (2020) Laparoscopic Treatment of a Patient with Perforated Jejunal Diverticulitis. J Med Res Surg. 1(3): pp. 1-4.
Copyright: ©2020 Buils Vilalta FJ, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits
unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Jejunal diverticular disease is a rare but important clinical entity. Jejunal diverticula usually remain asymptomatic in 60-70% of cases and cause symptoms or surgical complications in 10-19%. Perforation of a jejunal diverticulum is infrequent and treatment has traditionally been exploratory laparotomy, with resection of the affected intestinal segment. However, the laparoscopic approach can be a good alternative in these cases, providing the known advantages of this type of surgery. We present the case of a 75-year-old man who manifested himself as an acute abdomen and who was diagnosed and treated for a jejunal diverticulum perforation by laparoscopic surgery, with good results
Jejunal Diverticular, Laparoscopy, Peritonitis, Drilling
Jejunal diverticular disease is a rare clinical entity whose incidence ranges from 0.002 (in studies with small intestine contrast) to 4.6% (in studies performed by autopsy) [1]. These diverticula remain asymptomatic in 60-70% of cases and cause symptoms or surgical complications in 10-19% [2,3]. The preoperative diagnosis of jejunal diverticulitis is very rare and most of the time it is included in an acute abdomen picture [4]. Perforation of a jejunal diverticulum is infrequent and treatment has traditionally been exploratory laparotomy, with resection of the affected intestinal segment [5,6]. However, the laparoscopic approach [7] can be a good alternative in these cases, providing the known advantages of this type of surgery. The objective of the present study is to communicate our satisfactory experience in the laparoscopic treatment of a patient with a perforated jejunal diverticulum.
A 75-year-old man who attended the emergency department due to rectal bleeding without accompanying abdominal pain. His personal history included prostatectomy, obesity, Obstructive Sleep Apnea-Hypopnea Syndrome (OSAHS), arterial hypertension, arthroplasty due to left gonarthrosis, hyperuricemia, depressive syndrome, and colonic diverticulosis with two episodes of acute diverticulitis. Physical examination revealed cold and pale skin and mucosa, normal cardiopulmonary auscultation with 60 beats/min, blood pressure of 124/62 mmHg, and oxygen saturation of 97%. During the physical examination, only the presence of signs of bleeding was evident in the digital rectal examination. In the initial analytical study, neither leukocytosis nor left deviation was demonstrated. Hemoglobin levels were 9.5 g/dl, hematocrit (30.8%), urea (66mg/dl) and PCR of 2.6 mg/dl.
After clinical improvement and with the diagnosis of rectal bleeding secondary to colonic diverticulosis, he was admitted to hospital for evolutionary control. The patient presented a favorable evolution with the cessation of episodes of rectal bleeding. However, on the third day of admission, she debuted with a sudden onset of abdominal pain accompanied by a vasovagal picture, with defense and generalized peritoneal irritation. A new urgent analytical study revealed leukocytosis with left deviation, urea of 44.74 mg/dl, hemoglobin of 9.6 g/dl, hematocrit of 30.9% and a PCR of 1.2 mg/dl.
With the clinical suspicion of a complication of his diverticular disease, an urgent abdominal Computed Tomography (CT) was performed. CT showed a moderate amount of pneumoperitoneum and a discrete amount of free fluid, as well as the presence of diverticula throughout the colon and a large jejunal diverticulum (Figure 1). All this oriented to a possible microperforation of the transverse colon in the context of diverticular disease versus microperforation of the great jejunal diverticulum.
At this time, urgent surgical intervention was decided, performing a laparoscopic approach for both diagnostic and therapeutic purposes. A total of four trocars (10 mm optical trocar, two 5 mm trocars, and one 12 mm trocar) were used, with a moderate amount of purulent peritoneal exudate observed in the left subphrenic space, perisplenic, between loops and in the pelvic area. Likewise, a small perforation was revealed in the antimesenteric border of a large jejunal diverticulum, about 25 cm from the Treitz angle (Figure 2). After dissection and release of the diverticulum, resection of the diverticulum was performed at its base level with endogia (Figure 3). The postoperative period went smoothly and he was discharged on the 6th postoperative day. The pathological study confirmed that it was a jejunal diverticulum with perforation of its wall.
 Figure 1: Abdominal CT showing a large jejunal diverticulum (arrow) accompanied by pneumoperitoneum..
Figure 1: Abdominal CT showing a large jejunal diverticulum (arrow) accompanied by pneumoperitoneum..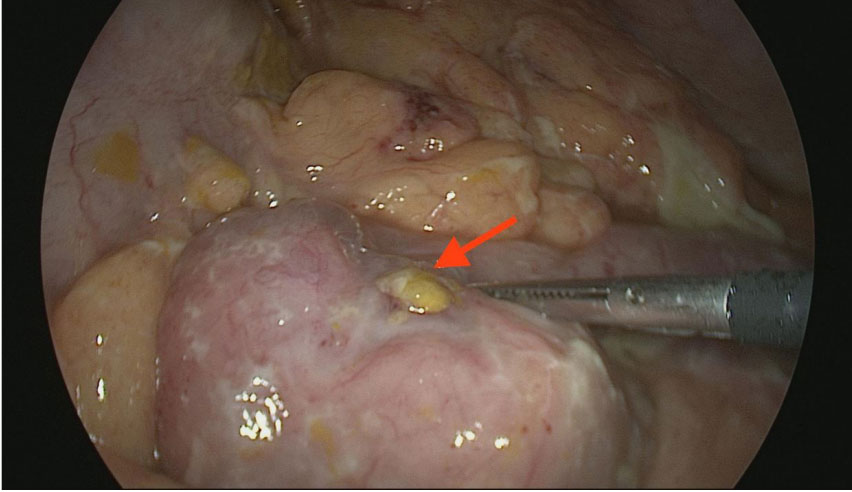 Figure 2: Result after the diverticulum section. The staple line can be seen on the left of the image and the diverticulum section on the right.
Figure 2: Result after the diverticulum section. The staple line can be seen on the left of the image and the diverticulum section on the right.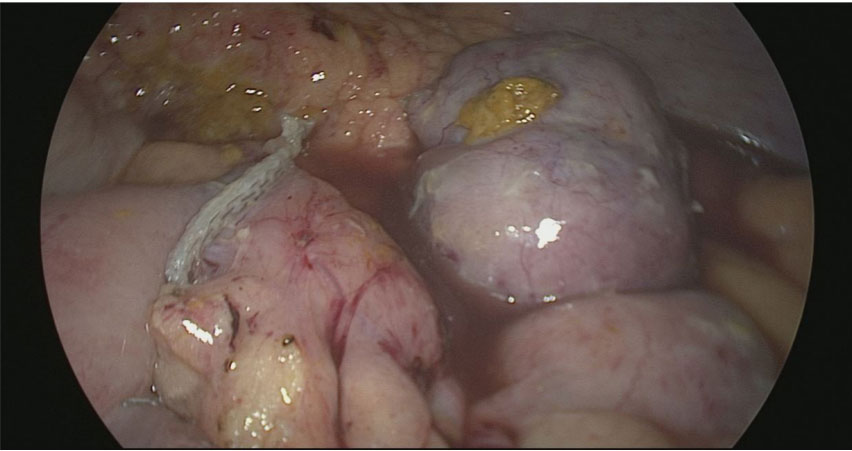 Figure 3: Result after the diverticulum section. The staple line can be seen on the left of the image and the diverticulum section on the right.
Figure 3: Result after the diverticulum section. The staple line can be seen on the left of the image and the diverticulum section on the right.The jejunal and ileum diverticula, together with the stomach, occupy the last place in the frequency of the digestive diverticula. Despite having been described as a defined anatomic entity for years, the epidemiology of intestinal diverticulosis is uncertain. As it is an acquired disease and is associated with a slow etiopathogenic process, it affects elderly people, with a peak incidence, as in our case, between the sixth and seventh decade of life. They are pulse diverticula and are caused, according to the most accepted hypothesis, by an increase in intraluminal pressure, as a consequence of uncoordinated intestinal contractions.
The local increase in intraluminal pressure would cause the mucosa and submucosa to protrude in the weakest area of the intestinal wall, just where the vessels of the mesentery penetrate, which would explain why the acquired diverticula settle in the mesenteric border of the intestine and are more frequent and bulky in the proximal jejunum, where the rectus vessels have a larger caliber. Most of the time, jejunal diverticula remain asymptomatic and only cause symptoms or surgical complications in 10-19% of cases. Therefore, the preoperative diagnosis of jejunal diverticulitis is very rare, but it must be taken into account in the presence of an acute abdominal condition [8]. CT can be very useful as a preoperative diagnostic tool in case of perforation and abscess [9]. In fact, in our case, this test allowed us to guide the diagnosis of a microperforation.
In the treatment of perforated jejunal diverticulitis, most authors advocate a cheap intestinal resection with primary anastomosis. However, some recommend extensive resections due to the possibility of future complications [4,10]. In our experience, the laparoscopic approach presents a good alternative in these cases. Garg et al, among others, also reported good results with this approach [11-13]. However, in these cases, the authors performed an intestinal resection of the affected segment and not a diverticulectomy as in the case we present. In our case, the laparoscopic approach allowed a certain diagnosis and an adequate and quick treatment, which also allowed the dissection and excision of the diverticulum without the need for intestinal resection. In summary, the laparoscopic approach of perforated jejunal diverticula is an option that, if you have the technical and human resources to carry it out, can be a great advantage for the treatment of this surgical complication. We believe that a laparoscopic approach is a tool that should be considered when faced with an acute abdomen, both in diagnostic and therapeutic management.
There are no conflicts of interest
