 Journal of Medical Research and Surgery
PROVIDES A UNIQUE PLATFORM TO PUBLISH ORIGINAL RESEARCH AND REMODEL THE KNOWLEDGE IN THE AREA OF MEDICAL AND SURGERY
Journal of Medical Research and Surgery
PROVIDES A UNIQUE PLATFORM TO PUBLISH ORIGINAL RESEARCH AND REMODEL THE KNOWLEDGE IN THE AREA OF MEDICAL AND SURGERY
 Journal of Medical Research and Surgery
PROVIDES A UNIQUE PLATFORM TO PUBLISH ORIGINAL RESEARCH AND REMODEL THE KNOWLEDGE IN THE AREA OF MEDICAL AND SURGERY
Journal of Medical Research and Surgery
PROVIDES A UNIQUE PLATFORM TO PUBLISH ORIGINAL RESEARCH AND REMODEL THE KNOWLEDGE IN THE AREA OF MEDICAL AND SURGERY
 Indexed Articles
Indexed ArticlesSelect your language of interest to view the total content in your interested language
Zahoor Ahmad Teli1, Shehnaz R. Kantharia2 , Aayushi Kantharia3, Rajesh A. Kantharia4*
, Aayushi Kantharia3, Rajesh A. Kantharia4*
1Junior Consultant, Head and Neck Surgical Oncology, Kailash Cancer Hospital & Research Centre, Muni Seva Ashram, Goraj, Vadodara, Gujarat,
India
2Consultant, Otorhinolaryngology, Head and Neck Surgery, Kailash Cancer Hospital & Research Centre, Muni Seva Ashram, Goraj, Vadodara,
Gujarat, India
3Final Year BDS Student, K M Shah Dental College and Hospital, Piparia, Waghodia, Vadodara, Gujarat, India
4Medical Director and Head, Department of Head and Neck Surgical Oncology, Kailash Cancer Hospital and Research Centre, Muni Seva Ashram,
Goraj, Vadodara, Gujarat, India
Correspondence to: Rajesh A. Kantharia, Medical Director and Head, Department of Head and Neck Surgical Oncology, Kailash Cancer Hospital and Research
Centre, Muni Seva Ashram, Goraj, Vadodara, Gujarat, India
Received date: July 09, 2022; Accepted date: July 20, 2022; Published date: July 27, 2022
Citation: Teli ZA, Kantharia SR, Kantharia A, et al. Head and Neck Schwannomas: Interesting Case Series with Review of Literature. J Med Res Surg. 2022; 3(4): 67-
70. doi:10.52916/jmrs224083
Copyright: ©2022 Teli ZA, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted
use, distribution and reproduction in any medium, provided the original author and source are credited.
Schwannoma is a benign, encapsulated and a slowly growing peripheral neural sheath tumor that arises from the schwann cells. 25-40% of Schwannomas occur in the head and neck region and of which 1-12% are seen in the oral cavity. The most common subsite in the oral cavity is tongue followed by the palate and buccal mucosa. The most commonly involved nerves include hypoglossal, lingual, tympanic, glossopharyngeal, vagus and the superior laryngeal nerves. The common presentation is a painless nodule or a swelling depending on the site of presentation. The preoperative diagnosis of schwannoma is usually suggested by Fine Needle Aspiration Cytology (FNAC) and is confirmed by histo-pathologic examination. The extent, exact location and relation with surrounding structures is delineated by imaging in the form of Ultrasound scanning, Computed Tomography (CT) scan or Magnetic Resonance Imaging (MRI). However, MRI is the imaging modality of choice as it provides better soft tissues details with precision along with the nerve of origin. Surgical excision is the treatment of choice. Recurrence is insignificant and has very rare chances of malignant transformation.
Head and neck schwannoma, Tongue schwannoma, Neurilemmoma, Extracapsular dissection, Ansa-cervacalis schwannoma
Schwannoma is a benign, encapsulated and a slowly growing peripheral neural sheath tumor that arises from the schwann cells. The nerves covered with schwann cells include cranial nerves (except the optic and olfactory nerves), spinal and autonomic system nerves [1]. 25-40% of Schwannomas occur in the head and neck region and of which 1-12% are seen in the oral cavity [2]. The most common subsite in the oral cavity is tongue followed by the palate and buccal mucosa [3,4]. The most commonly involved nerves include hypoglossal, lingual, tympanic, the glossopharyngeal, vagus and the superior laryngeal nerves.
The gold standard for treatment of Schwannomas in majority of cases is surgical resection. The recurrence rate is very low with rare chances of malignant transformation [5]. We present two case reports of schwannomas, 1) involving the left lateral border of tongue originating from lingual nerve and 2) from left neck arising from ansa-cervacalis.
A 52 years old male patient reported to the Department of Head and Neck Surgical Oncology, Kailash Cancer Hospital and Research Centre with the chief complaints of swelling on the left lateral border of tongue for 2 years. On clinical examination, a submucosal nodule measuring 3.5 × 3.5 cm in size, elastic to firm in consistency, was present on the latero-ventral aspect of left side of tongue. The overlying mucosa was ulcerated from last 10 days for which he sought medical opinion. Floor of mouth was free. The patient felt slight pain for the last one week which was relieved by medication. There was no hypoglossal or lingual nerve paralysis. Fine Needle Aspiration Cytology (FNAC) was done which was negative for malignancy. MRI of oral cavity and neck was done to further evaluate the extent and exact location of the lesion. MRI showed a 4.8 × 4.6 × 3.9 cm (AP × TRA × CC) size peripherally enhancing centrally cystic mass lesion with irregular enhancing wall on the left lateral border of tongue which was going into the base of tongue, mostly suggestive of a benign pathology as shown in (Figure 1). Complete extracapsular excision was done under general anaesthesia as shown in (Figure 2). During surgical excision the tumor was in close association with lingual nerve which was dissected and preserved. The final histopathological report showed a diagnosis of benign spindle cell neoplasm consistent with schwannoma. The post-operative healing was uneventful and the patient was followed for 6 months. The patient did not show any signs of nerve injury during the course of recovery and follow up. The microscopic photograph of various resolutions is shown in (Figure 3).
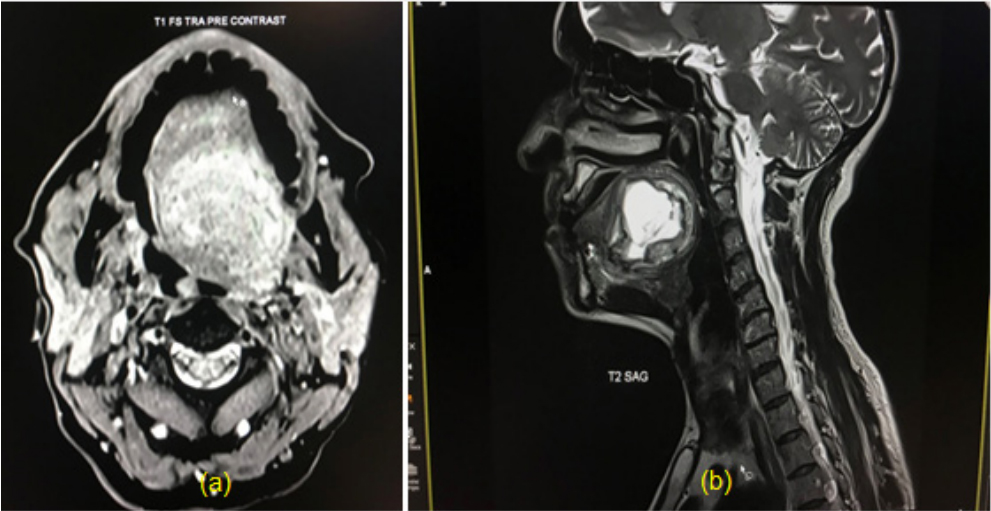 Figure 1: MRI images of tongue schwannoma; a): T1 weighted MRI image
showing isointense to hypointense homogenously enhancing lesion and
hyperinterse homogenous lesion on T2 weighted image on the left lateral
border of tongue; b): Post contrast MRI showed a 4.8 × 4.6 × 3.9 cm (AP × TRA
× CC), size peripherally enhancing centrally cystic mass lesion with irregular
enhancing wall on the left lateral border of tongue which was going into the
base of tongue.
Figure 1: MRI images of tongue schwannoma; a): T1 weighted MRI image
showing isointense to hypointense homogenously enhancing lesion and
hyperinterse homogenous lesion on T2 weighted image on the left lateral
border of tongue; b): Post contrast MRI showed a 4.8 × 4.6 × 3.9 cm (AP × TRA
× CC), size peripherally enhancing centrally cystic mass lesion with irregular
enhancing wall on the left lateral border of tongue which was going into the
base of tongue. 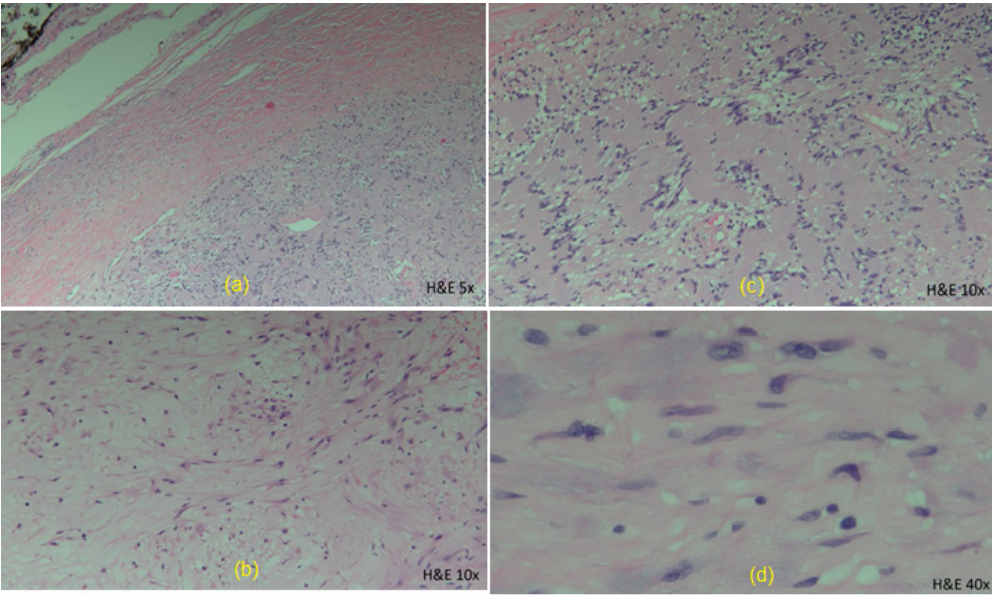 Figure 3: a): Photograph of histopathological section (H and E, 5X) Low
power view showing a part of a capsulated spindle cell tumor; b): (H and E, 10X: Hypercellular area of the tumor with verrocay bodies; c): (H and E, 10X): Hypocellular area of the tumor with spindled tumor cells set within a myxoid stroma; d): (H and E, 40X): High power view with spindled tumor cells
displaying wavy and buckled nuclei.
Figure 3: a): Photograph of histopathological section (H and E, 5X) Low
power view showing a part of a capsulated spindle cell tumor; b): (H and E, 10X: Hypercellular area of the tumor with verrocay bodies; c): (H and E, 10X): Hypocellular area of the tumor with spindled tumor cells set within a myxoid stroma; d): (H and E, 40X): High power view with spindled tumor cells
displaying wavy and buckled nuclei.A 30 years old male patient reported to the Department of Head and Neck Surgical Oncology, Kailash Cancer Hospital and Research Centre with the chief complaints of swelling on the left upper side of neck for 3 years. On clinical examination, a solid mass measuring 5 × 5 cm in size, firm to hard in consistency, was present on the left side of neck at the level of upper and middle part of Internal Jugular Vein (IJV). The overlying skin surface was normal. The remainder of ENT examination was unremarkable. Trucut biopsy was done which showed a diagnosis of low grade spindle cell neoplasm favouring schwannoma. MRI of oral cavity and neck was done to further evaluate the extent and exact location of the lesion. MRI showed a Large, well-defined heterogeneously enhancing solid lesion at left level II and III involving carotid space, measuring 4 × 5.4 × 7.8 cm (AP × TRA × CC). It appeared heterogeneously hyper intense on T2WI/STIR, hypo intense on T1WI, and showed internal non enhancing area. It was posterior to the carotid space and displaced the left IJV, common carotid and carotid bifurcation anteriorly. The left IJV, was not visualized mostly due to compression by the mass. The mass abutted common carotid artery and its branches with no evidence of encasement/ infiltration of artery. Laterally, it abutted left sterno-cleido mastoid muscle with no infiltration seen. Postero-medially, it abutted peri vertebral muscles with no infiltration seen as shown in (Figure 4). MRI Angiography showed normal contrast opacification in left carotid arterial system. Surgical excision of the lesion was done under general anaesthesia as shown in (Figure 5). During excision the tumor was in close association with ansa cervicalis which was dissected and preserved. The final Histopathological report showed a confirmative diagnosis of schwannoma. The postoperative healing was uneventful and the patient was followed for 9 months. The patient did not show any signs of nerve injury during the course of recovery and follow up.
Schwannomas are benign encapsulated slowly growing tumors that originate from the Schwann cells of the nerve sheath and was first reported by verocay in 1910 [6]. Schwann cells are neural crest-derived glial cells that are responsible for providing myelin insulation to peripheral nervous system axons. Schwannomas (Neurilemmoma) are commonly seen in head and neck region with literature reporting cases seen also along the flexor surfaces of the peripheral extremities. Intraoral schwannomas are rare which mostly occur on tongue followed by palate, floor of the mouth, buccal mucosa, gingiva, lips and the vestibular mucosa [7]. Most of the literature shows no gender or race predilection and can occur throughout a wide age range. Most commonly schwannomas occur between second to 4th decade of life [8,9].
Schwannomas are slowly growing tumors with usually long onset before presentation. The mean duration of the disease is usually around 3 years [10,11]. In the present case series the mean duration was around 2 and half years. The common presentation is a painless nodule or a swelling depending on the site of presentation [12]. Butler et al., in his retrospective study on the clinicopathological features of schwannomas over a period of 20 years showed that most of the cases were asymptomatic with local symptoms seen only in oral and laryngeal tumors with increase in the size and neurological symptoms were seen in tumors adjacent to or within the bone [13].
The preoperative diagnosis of schwannoma is usually suggested by FNAC and is confirmed by histo-pathologic examination [14]. Liu et al., reported that the accuracy of FNAC was only 20% and it is difficult to characterize on FNAC [15]. The extent, exact location and relation with surrounding structures is delineated by imaging in the form of Ultrasound scanning, CT scan or an MRI. In non contrast CT scan the schwannomas present as well circumscribed, dense and homogenous soft tissue masses [16]. However, MRI is preferred and the imaging modality of choice as it better delineates the soft tissue components with the nerve of origin. In MRI the tumor appears as a smooth and well demarcated lesion which is iso-intense or hypointense to muscle on T1 weighted images and homogenously hyperintense on T2 weighted images [17]. In the present case series MRI was done in both the cases. Hirano et al. reported that MRI was useful for the diagnosis of head and neck schwannomas and showed peripheral hyperintense rim with central low intensity on enhanced T1 images of MRI [18]. The relationship between the schwannoma and its nerve of origin can be better appreciated with MRI than CT scan and is most sensitive and specific in the diagnosis of schwannomas [19].
The differential diagnosis of schwannoma include traumatic neuroma, ganglioneuroma, solitary circumscribed neuroma, mucosal neuroma, , granular cell tumours, hemangiomas, leiomyomas, rhabdomyomas, lymphangiomas, irritation fibromas, lipomas, pyogenic granulomas and benign salivary gland tumours [20]. Schwannomas can occur alone or as a part of genetically inherited diseases like Neufibromatosis (NF) type 1 and type 2 and schwannomatosis. The hallmark signs of NF type 2 are vestibular schwannomas, whereas in case of schwannomatosis, which is a form of NF type 2, these tumours are absent [21].
Total surgical excision is the treatment of choice. In case of tongue lesion, transoral approach was used for excision of the tumor. Extra-capsular dissection was done and Lingual nerve was seen closely associated with the lesion, for which blunt dissection was done and preserved as shown in (Figure 2). In case of neck Schwannoma, transcervical approach was used and the mass was seen abutting the structures in the carotid space. Extracapsular dissection was done with careful preservation of common carotid artery along with the branches, IJV and the vagus nerve as shown in (Figure 5). The mass was seen associated and originating from ansa-cervicalis which was dissected and preserved. There was no post-operative nerve palsy in both the cases and healing was uneventful. Schwannomas don’t recur and if it does could be due to incomplete surgical excision [22]. Schwannomas are radio-resistant tumors. Malignant transformation of schwannomas in general is unusual and very rare, however, Enoz etal in his study reported a transformation rate of 8-10% for head and neck schwannomas [16].
Final histopathology is confirmative for the diagnosis of schwannomas. Most of the head and neck Schwannomas are encapsulated. Histologically, it presents as alternating pattern of Antoni A or Antoni B. Antoni A is hypercellular composed of spindle cells arranged in waves, drifts and whorls with nuclear palisading leading to formation of verocay bodies (nuclear palisading around a collagenous hylanised core or around a central mass of cytoplasm). Antoni B pattern is made up of very loose tissue, lacking the arrangement in the bundle and palisades, and is hypocellular composed mainly of round cells separated by abundant myxoid, often microcystic matrix [23]. Schwannomas are characterised by positive immunohistochemical markers like S-100 and SOX10 [24].
Head and neck schwannoma is an asymptomatic, slowly growing benign tumor presenting as a well circumscribed nodule with typical signal and dynamic characteristics. Surgical excision is the treatment of choice. Recurrence is insignificant and has very rare chances of malignant transformation.
This study was approved by the Institutional Review Board (IRB) of Kailash Cancer Hospital and Research Centre and all participants signed an informed consent agreement.
Patients have signed an informed consent form separately for photographs to be used for research purposes and for publication in the journals.
All data and materials related to the study is available to review.
None.
The authors declare no competing financial interest.
None
