 Journal of Medical Research and Surgery
PROVIDES A UNIQUE PLATFORM TO PUBLISH ORIGINAL RESEARCH AND REMODEL THE KNOWLEDGE IN THE AREA OF MEDICAL AND SURGERY
Journal of Medical Research and Surgery
PROVIDES A UNIQUE PLATFORM TO PUBLISH ORIGINAL RESEARCH AND REMODEL THE KNOWLEDGE IN THE AREA OF MEDICAL AND SURGERY
 Journal of Medical Research and Surgery
PROVIDES A UNIQUE PLATFORM TO PUBLISH ORIGINAL RESEARCH AND REMODEL THE KNOWLEDGE IN THE AREA OF MEDICAL AND SURGERY
Journal of Medical Research and Surgery
PROVIDES A UNIQUE PLATFORM TO PUBLISH ORIGINAL RESEARCH AND REMODEL THE KNOWLEDGE IN THE AREA OF MEDICAL AND SURGERY
 Indexed Articles
Indexed ArticlesSelect your language of interest to view the total content in your interested language
Gohar Ali* , Jawad Ali, Fazal Ullah, Muhammad Tayyab Khan
, Jawad Ali, Fazal Ullah, Muhammad Tayyab Khan  , Muhammad Kashif Dawar, Shandana Khan, Anees Ahmed
, Muhammad Kashif Dawar, Shandana Khan, Anees Ahmed
Department of General Surgery, Hayatabad Medical complex, Peshawar, Pakistan.
Correspondence to: Gohar Ali, Department of General Surgery, Hayatabad Medical complex, Peshawar, Pakistan.
Received date: January 04, 2025; Accepted date: January 27, 2025; Published date: February 02, 2025
Citation: Ali G, Ali J, Ullah F, et al. Frequency of Port Site Infection in Laparoscopic Cholecystectomy, Evaluation by Southampton Score: A Prospective Study. J Med Res Surg. 2025;6(1):9-14. doi: 10.52916/jmrs254158
Copyright: ©2025 Ali G, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Objective: To evaluate the frequency of Port-Site Infections (PSIs) following Laparoscopic Cholecystectomy (LC) using the Southampton Scoring System and identify associated risk factors. Methodology: This prospective cross-sectional study was conducted over two years in the Department of General Surgery at Hayatabad Medical Complex, Peshawar. Data were collected using a standardized proforma and analyzed using IBM SPSS version 23.0, with a significance value set at p<0.05. The Southampton Scoring System was used to monitor and grade wound infections at discharge, 2nd week and 4th weeks post-surgery. Results: After exclusion, 841 patients were included in the study, with 471 males (56%) and 370 females (44%). The average age was 45.9 ± 12.7 years. Significant intraoperative findings included symptomatic gallbladder stones (82.5%), acute cholecystitis (26%), thick-walled gallbladder (44.4%), bile spillage into peritoneum (41.5%), and gallbladder perforation (54.6%). The frequency of port site infection with Southampton scores of 3 and above was 9.9% for the umbilical port and 27.3% for the epigastric port. Significant risk factors for SSI included symptomatic gallbladder stones, acute cholecystitis, gangrenous gallbladder, spillage into the wound, gallbladder perforation, and surgery duration exceeding 90 minutes (p<0.05). Conclusions: The Southampton Scoring System effectively identified and tracked wound infections, underscoring the need for meticulous surgical techniques and thorough postoperative care to reduce SSIs. Although wound healing was initially good, complications increased by the 2nd and 3rd week, especially at the epigastric port. Most patients show significant improvement of wound healing by 4th week. Regular monitoring and timely interventions are essential to lower SSI rates in laparoscopic surgeries.
Laparoscopic cholecystectomy, Port site infection, Surgical Site Infection (SSI), Southampton Scoring, Risk factor.
Laparoscopic surgery has changed the modern surgical practice with minimally invasive procedures, reducing the post operative complications like pain, shortens recovery, early mobilization and low risks of infected wounds [1]. The incidence of major complications following laparoscopic procedures is notably low, around 1.4 per 1,000 surgeries, demonstrating the safety and effectiveness of laparoscopic techniques and solidifying their role as a cornerstone in contemporary surgical care [1-3]. During laparoscopic procedures, port-site complications, particularly surgical site infections, are common and include bleeding, hernias, emphysema, and hypertrophic scars [1]. Post-operative wound infection is defined as surgical site infection from 0-30 days after surgery, or infection to surgical site till one year in cases of implants like mesh, vascular grafts and prosthesis. In this context, after cholecystectomy, patients are undergoing clinical follow-up for wound examination, with wound sites classified according to the Southampton Scoring System [4]. The infection rate after clean surgery is a key indicator of surgical performance [5]. The Southampton Scoring System identifies grading surgical wounds infections and healing, furthermore, feedback on post-surgical wound status is crucial for reducing the risk of surgical site infections [6]. Therefore, we aimed to evaluate the usefulness of the Southampton Scoring System in assessing post-surgical wounds following wound status for 1 month.
It is a prospective cross-sectional study conducted in the Department of General Surgery at Hayatabad Medical Complex, Peshawar, over a minimum duration of two years following the approval by ethical committee. The sample size consists of 841 patients undergone laparoscopic cholecystectomy, using a convenient sampling technique. Consent was obtained from all the patients participated. Data collection was carried out using a standardized proforma. The collected data was analyzed using IBM SPSS version 23.0, with a significance value set at a p-value of 0.05 or lower. The analysis includes the student t-test and Pearson chi-square test. Southampton grading was frequently noted during follow-up for 1 month and they were monitored for surgical site infection in grades. Wounds were assessed clinically one week after surgery and, in cases of infection, were monitored weekly for up to four weeks in the outpatient clinic. All wound infections were treated with regular local washes and empirical oral antibiotics. The frequency of port site infections was analyzed concerning the extent of infection by Southampton score, duration of surgery, operative findings, and the site of the infected port. Additionally, we analyzed the following factors in relation to port site infections: symptomatic gallbladder stones, past history of cholecystitis, past history of pancreatitis, past history of surgery, ultrasound findings of acute cholecystitis, thick-walled gallbladder, adhesions, gangrenous gallbladder, bile spillage, perforation of the gallbladder, retrieval of the gallbladder in a bag, placement of a drain, spillage into the wound or bag tear, and whether the wound was washed.
All patients who were qualified for laparoscopic cholecystectomy like acute calculus cholecystitis, GB perforation, gangrenous GB, GB stones manifesting with Acute right upper abdominal pain.
Patients with loss of follow-up, conversion to open surgery, malignant and acalculous gallbladder.
Out of 1095 laparoscopic cholecystectomies, 841 were taken in sample, 254 were excluded from the study on basis of exclusion criteria shown in Figure 1. The study Includes Male 471 (56%) and Female 370 (44%). Table 1 shows the average age is 45.95 years with a standard deviation of 12.77 years, indicating moderate age variability. The median age is 47 years, and the most common age (mode) is 44 years. The data is approximately symmetric, with a slight left skewness of -0.079. Age range from a minimum of 24 years to a maximum of 72 years. Table 1 shows the majority of patients had symptomatic gallbladder stones (82.5%), with a significant number presenting with acute cholecystitis on ultrasound (26%) and thick-walled gallbladders (44.4%). Notable intraoperative findings included bile spillage in 41.5% of cases and gallbladder perforation in 54.6% of cases. Postoperative complications were prevalent, with wound washing required in 75.7% of cases, and the duration of surgery exceeding 90 minutes in 57.6% of patients.
Table 1: Baseline characteristics of the study population and frequency of infections.|
Features |
n (%) |
USSI (9.9%) |
ESSI (27.3%) |
|
Age (years) Mean ± SD |
45.9 ± 12.7 |
|
|
|
Gender |
|
|
|
|
Male |
471 (56%) |
45 (9.6%) |
165 (35%) |
|
Female |
370 (44%) |
38 (10.3%) |
65 (17.6%) |
|
Comorbidities |
|
|
|
|
None |
399 (47.4%) |
10 (2.5%) |
71 (17.8%) |
|
Diabetic |
306 (36.4%) |
73 (23.9%) |
51 (16.7%) |
|
Hypertensive |
85 (10.1%) |
0 (0%) |
57 (67.1%) |
|
Others comorbidity |
51 (6.1%) |
0 (0%) |
51 (100%) |
|
Symptomatic GB Stones |
694 (82.5%) |
83 (12%) |
230 (33.1%) |
|
Past Hx of Cholecystitis |
179 (21.3%) |
33 (18.4%) |
116 (64.8%) |
|
Past Hx of Pancreatitis |
34 (4%) |
0 (0%) |
17 (50%) |
|
Past Hx of Surgery |
0 (0%) |
83 (100%) |
210 (100%) |
|
US Acute Cholecystitis |
219 (26%) |
44 (20.1%) |
16 (7.3%) |
|
Thick Wall GB |
373 (44.4%) |
39 (10.5%) |
210 (56.3%) |
|
Adhesions |
85 (10.1%) |
0 (0%) |
34 (40%) |
|
Gangrenous GB |
35 (4.2%) |
15 (42.9%) |
13 (37.1%) |
|
Bile Spillage into wound |
350 (41.5%) |
48 (13.7%) |
139 (39.7%) |
|
Perforation of GB |
459 (54.6%) |
65 (14.2%) |
102 (22.2%) |
|
Retrieval of GB in bag |
231 (27.5%) |
3 (1.3%) |
5 (2.2%) |
|
Spillage into Wound/bag tear |
626 (74.4%) |
83 (13.3%) |
98 (15.7%) |
|
Wound washed yes |
637 (75.7%) |
19 (3%) |
165 (25.9%) |
|
Duration of Surgery (>90min) |
484 (57.6%) |
30 (6.2%) |
55 (11.4%) |
The frequency of port site infection with Southampton scores of 3 and more is 83 (9.9%) for the umbilical port and 230 (27.3%) for the epigastric port, resulting in a total of 313 (37.2%) infections.
Table 2: Southampton wound grading scores at different follow-up points.|
Umbilical port site infection |
|||
|
Southampton Score |
Discharge n (%) |
2nd Week n (%) |
4th Week n (%) |
|
0 |
351 (41.7 %) |
532 63.3% |
511 60.8% |
|
1 |
440 (52.3%) |
102 12.1% |
272 32.3% |
|
2 |
50 (5.9%) |
124 14.7% |
58 6.9% |
|
3 |
0 (%) |
83 9.9% |
n (%) |
|
4 |
0 (%) |
0 (%) |
n (%) |
|
5 |
0 (%) |
n (%) |
n (%) |
|
Epigastric port site infection |
|||
|
Southampton Score |
Discharge n (%) |
2nd Week n (%) |
4th Week n (%) |
|
0 |
230 27.3% |
466 55.4% |
500 59.5% |
|
1 |
254 30.2% |
48 5.7% |
203 24.1% |
|
2 |
357 42.4% |
97 11.5% |
138 16.4% |
|
3 |
0 (%) |
97 11.5% |
|
|
4 |
0 (%) |
133 15.8% |
|
|
5 |
0 (%) |
|
|
Table 2 summarizes the Southampton wound grading scores at discharge, 2nd week, and 4th week for umbilical port and epigastric port site infection. Table 2 show the distribution of Southampton scores for both the umbilical and epigastric ports were assessed at discharge, the 2nd week, and the 4th week post-surgery. At discharge, most patients had Southampton scores of 0 or 1 for both the umbilical and epigastric ports, indicating fewer wound infections. By the 2nd week, scores of 2 and 3 increased, especially for the epigastric port, suggesting more wound complications. However, by the 4th week, most patients improved significantly, with the majority having a score of 0, indicating good wound healing.
Despite this, the epigastric port still had several patients with higher scores, reflecting some ongoing complications. Our study evaluated by the Southampton score, revealed that while initial wound healing was generally good, a significant increase in wound complications was observed by the 2nd week, particularly at the epigastric port. By the 4th week, most patients showed substantial improvement, with the majority having minimal or no infections.
Table 3: Analysis of Risk Factors for SSI.|
Variable |
SSI (n, %) |
p-value |
|
Symptomatic GB Stones |
313(100%) |
0.00 |
|
US Acute Cholecystitis |
60(19.1%) |
0.00 |
|
Gangrenous GB |
28(8.9%) |
0.00 |
|
Spillage into Wound |
177(56.5%) |
0.00 |
|
Perforation of GB |
187(59.7%) |
0.00 |
|
Duration of Surgery>90 mins |
182(58.1%) |
0.00 |
Table 3 highlights significant risk factors for Surgical Site Infection (SSI) in patients undergoing gallbladder surgery. Key factors include symptomatic gallbladder stones (100%), acute cholecystitis (19.1%), gangrenous gallbladder (8.9%), spillage into the wound (56.5%), gallbladder perforation (59.7%), and In Figure 2 and 3:
For the umbilical port site infections, the majority of cases had a Southampton score of 0 at discharge (41.7%), with an increase to 63.3% by the 2nd week and 60.8% by the 4th week, indicating effective healing over time. Cases with a score of 1 showed a decrease from 52.3% at discharge to 12.1% at the 2nd week, with a slight increase to 32.3% at the 4thweek. Higher scores (2-5) were relatively rare, with minimal or no cases beyond the 4th week.
Our statistical analysis identified several significant risk factors for Surgical Site Infections (SSI), using chi square test, including symptomatic gallbladder stones (100%), acute cholecystitis (19.1%), gangrenous gallbladder (8.9%), spillage into the wound (56.5%), perforation of the gallbladder (59.7%), and a surgery duration of more than 90 minutes (58.1%) (p-value<0.05 for all).
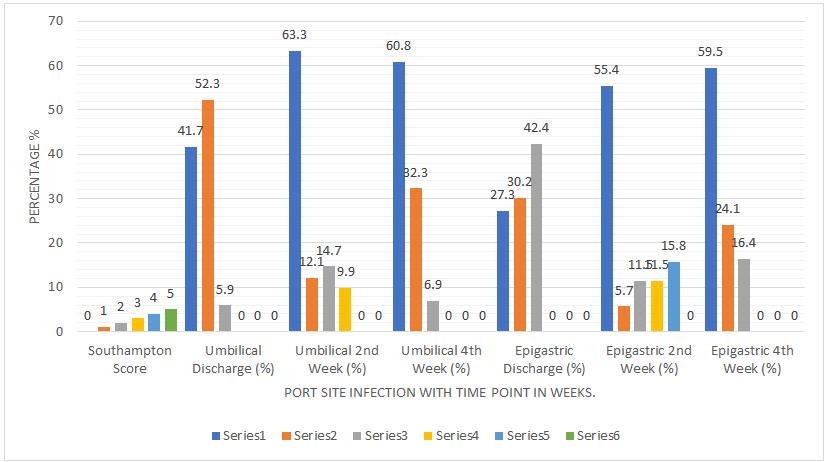 Figure 2: Comparison of umbilical and epigastric port site infection frequencies by southampton scores at different follow-up points.
Figure 2: Comparison of umbilical and epigastric port site infection frequencies by southampton scores at different follow-up points.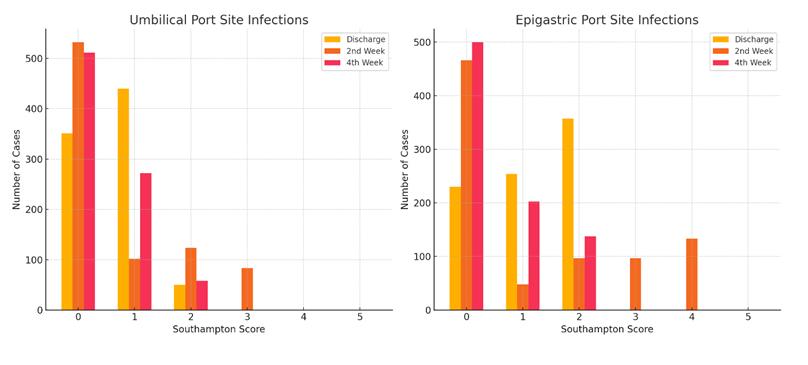 Figure 3: Distribution of epigastric port site infections by southampton scores at discharge, 2nd week, and 4th week.
Figure 3: Distribution of epigastric port site infections by southampton scores at discharge, 2nd week, and 4th week.Laparoscopic cholecystectomy is safe, effective and innovative procedure despite its complications, including port site infections, it is the standard of care for gallbladder stones discussed in literature such as Sasmal et al, Paterson-Brown S. et al. and Z Holub [7-9]. Different studies shows port-site infection in range of 2.4% to 6.7% mentioned by Mohd Altaf Mir et al. and D Saud jasim et al. [10,11]. Our study in contrast shows high rate of infections 0% in 1st week, 37.3% in 2nd week and 0% in 4th week following the same patients stating that Southampton score of 3 or more is infective. Additionally, there were 15.8% infection rate with Southampton score of 4. Differences in environment, population, and sterilization techniques between hospitals, along with rapid turnover, may impact infection rates. Our reasons of high rate of infections might be the reusable trocars.
Epigastric port was most commonly infected in our study, similar findings of Jan et al. and Mohd Altaf [10,12]. Colizza et al., Hamzaoglu et al. and Tocchi et al. in contrast shows that umbilical port is most commonly infected [13-15]. In our study frequent infection of epigastric port may be due to frequent retrieval of gall bladder through epigastric port. Jenishkumar Vijaykumar et al. shows there is no diffrenece in infections of port site either retrieval through epigastric or umbilical port [16].
In our study, patients with symptomatic gallbladder stones, as well as those with a history of acute or past cholecystitis were most commonly linked to port site infections with higher Southampton scores (grades 2 and 3). Similar findings have been reported in studies by Chuang Shih-Chang et al. [17,18].
Bile spillage into the peritoneum is identified as a risk factor for port site infection, according to studies by Peponis Thomas et al. and Mehmood Yasir et al. [19,20]. Our study demonstrates that patients with a bile spillage during gallbladder perforation tend to have a higher incidence of infections at the epigastric port site, with scores of 4 and 3 being most frequent.
Gangrenous gall bladder, thick wall GB and adhesions of GB shows lower rate of infections while these are significant risk factors in our study. In litrature our study is similar to Md Rezaul Alam et al. [21] we have experienced that thick wall gallbladder and adhesions of GB with surrounding structures may prolong the duration of surgery which is significant risk factor.
We were able to see a significant relation between duration of surgery and PSIs. However, we kept our time of surgery range below 90 minutes and above 90 minutes. The longer the length of surgery the more is PSIs and higher the Southampton score in 2nd week. Similar studies by Md Rezaul Alam et al. and Anielski et al. but with different range of time [21,22].
Bile spillage during retrieval or bag tears can lead to frequent port site infections. However, our study shows that retrieving the gallbladder in a bag or preventing wound spillage lowers infection rates. Dugg Pankaj et al., Sasmal Prakash K et al., and Mehmood Yasir et al. found that using an endobag decreases port site infections. An improvised endobag from a surgical glove is effective, cheap, and disposable [7,19,23].
Our study identified a significant frequency of PSIs in LC using the Southampton Scoring System, with higher rates observed at the epigastric port compared to the umbilical port. Additionally, the study indicates a significant reduction in port site infections from discharge to the fourth week, with most infections being mild and severe infections remaining relatively rare at both umbilical and epigastric port sites.
The Southampton Scoring System effectively identified and monitored wound infections following LC, emphasizing the need for meticulous surgical technique and postoperative care to minimize SSIs. Despite initial good wound healing, a significant increase in wound complications was observed by the second week, particularly at the epigastric port. By the 4th week, most patients showed substantial improvement. Continuous monitoring and appropriate interventions are crucial for reducing SSI rates in laparoscopic procedures. LC has a low risk of infection of port-site which is just superficial responding to local measures.
Our study was limited by its single-center design, which may restrict the generalizability of findings to other Institutes. And Southampton score of greater than was clinically decided to be in range of infections, otherwise it should be confirm by culture of the wound discharge. Additionally, follow-up was limited to four weeks post-surgery, which may not capture longer-term complications.
Ethical approval for the study was obtained from the Institutional Review Board of Hayatabad Medical Complex, Peshawar. Our IREB Number is 1926.
Written informed consent was obtained from all participants prior to their inclusion in the study.
The authors wish to thank the Department of Surgery of their institution for making the present work possible.
No financial support was received in relation to this article.
The authors declare that there is no conflict of interest.
