 Journal of Medical Research and Surgery
PROVIDES A UNIQUE PLATFORM TO PUBLISH ORIGINAL RESEARCH AND REMODEL THE KNOWLEDGE IN THE AREA OF MEDICAL AND SURGERY
Journal of Medical Research and Surgery
PROVIDES A UNIQUE PLATFORM TO PUBLISH ORIGINAL RESEARCH AND REMODEL THE KNOWLEDGE IN THE AREA OF MEDICAL AND SURGERY
 Journal of Medical Research and Surgery
PROVIDES A UNIQUE PLATFORM TO PUBLISH ORIGINAL RESEARCH AND REMODEL THE KNOWLEDGE IN THE AREA OF MEDICAL AND SURGERY
Journal of Medical Research and Surgery
PROVIDES A UNIQUE PLATFORM TO PUBLISH ORIGINAL RESEARCH AND REMODEL THE KNOWLEDGE IN THE AREA OF MEDICAL AND SURGERY
 Indexed Articles
Indexed ArticlesSelect your language of interest to view the total content in your interested language
Correspondence to: Naveen Kumar, Department of Burns, Plastic and Reconstructive Surgery, PGIMER, New Delhi -110001; E-mail: drnaveenvmmc@gmail.com
Received date: January 9, 2020; Accepted date: January 18, 2020; Published date: January 25, 2020
Citation: Kumar A, Kumar N, Lal R, et al. (2020) Experience of Component Separation Technique with Open Posterior and Endoscopic Assisted Laproscopic Approach in the Management of Large Midline Ventral Hernias. J Med Res Surg 1(1): pp. 1-8.
Copyright: © 2020 Kumar A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Background: A novel technique of posterior component separation using transversus abdominis release has been propagated to recreate the midline (Linea alba) in patients with large midline incisional hernias and provides a large space for placement of an underlay mesh. Another recent technique popularized by minimal access surgeons is the endoscopically assisted anterior Component Separation Technique with laparoscopic intra-abdominal composite mesh repair.
Method: In our study, we did open Component separation by the posterior approach for the first fifteen patients and Endoscopic assisted component separation with laparoscopic meshplasty for the next fifteen patients. A minimum component separation index from the data of the first fifteen patients was calculated using pre-operative CECT scans validating the requirement of component separation index the endoscopic group of patients. All the repairs were reinforced using a prolene or composite mesh as a standard practice.
Result: The wound complications were more with the open technique while the endoscopic procedure was associated with lesser blood loss and faster post-operative recovery. Improved functional and cosmetic outcomes were observed in both groups.
Conclusion: The component separation done by either a posterior open or endoscopic technique results in good functional and cosmetic outcomes for the patients with no reported recurrences.
Component separation; Ventral hernia; Endoscopic; Posterior open; Transverse abdominis
CST: Component Separation Technique; CSI: Component Separation Index; CECT: Contrast-Enhanced Computed Tomography; MDCT: Multi-detector Computed Tomography
Incisional hernia is a post-operative complication characterized by the escape of the abdominal viscera from their anatomic site through a hole developed during the cicatricial consolidation of a laparotomy [1]. The field of abdominal wall reconstruction surgery continues to evolve to improve the outcome, eliminate the risk of wound complications and hernia recurrence. Closure of small midline defects is most often accomplished with medial advancement of adjacent abdominal wall structures, provided that these tissues are available, well-vascularized, and mobile, i.e., not fixed by cicatrix or scar [2]. When large full-thickness abdominal wall defects are present, autogenous tissue options include the transposition of local or regional musculocutaneous or musculofascial flaps and, occasionally, the provision of a free flap transfer. Ramirez et al. [3] developed a technique for reconstructing abdominal wall defects without the use of prosthetic material.
Presently different ways of performing CST include:
The classical anterior component separation involves elevation of large subcutaneous flaps to provide access to the lateral abdominal wall musculature. However, extensive dissection can result in skin flap necrosis, seroma, hematoma, and massive wound infections [4]. Recently a novel technique of posterior component separation using Transversus Abdominis Release (TAR) has been propagated to recreate the midline (Linea alba) in patients with large midline incisional hernias and provides a large space for placement of an underlay mesh [5]. Another recent technique popularized by minimal access surgeons is the endoscopically assisted anterior CST with laparoscopic intra-abdominal composite mesh repair. The use of endoscopy provides multiple surgical advantages, including decreased scarring, preservation of anatomic structures, and decreased morbidity. Endoscopy is associated with less postoperative pain, more rapid recovery and consequentially, a diminished length of hospital stay and reduced overall cost of repair [6].
We expect the present proposed study will help gather more information regarding the outcome of a component separation technique and supplement the data regarding the same so that more definitive guidelines can be formulated for the future.
The prospective observational study was conducted from December 2013 to March 2016. A convenient sample size of 90 patients attending the Surgery out Patient Department (OPD) and having clinical features of incisional hernias constituted the study population. Inclusion Criteria included patients of age between 18 years and 80 years with the diagnosis of incisional hernia, midline incisional hernias, good performance status (ASA-I&II). Exclusion criteria included patients with lateral or paramedian incisional hernias, pregnant and lactating patients, patients having a stoma, patients with severe respiratory or cardiac co-morbidities (ASA: III-V). Study Materials included a Multidetector CT Machine, Laparoscopic Spacemaker Balloon for creating space to facilitate endoscopic CST, Polypropylene mesh and Composite mesh
The study included 90 patients of incisional hernias who underwent component separation by either open or endoscopically assisted laparoscopic technique under general anesthesia.
Routine investigations or were done. Cardiac and pulmonary status was evaluated. A pre-operative CECT was done for each patient and the size, location of the defect along with the Component Separation Index (CSI) was assessed. Initially, all patients were taken up for open hernioplasty. They were assessed for defect size and ability to close the defect with or without tension.
After a complete adhesinolysis via a generous midline laparotomy, the posterior rectus sheath was incised about 0.5–1 cm from its medial edge. The retrorectus plane was then developed towards the Linea semilunaris. Starting in the upper third of the abdomen, about 0.5 cm medial to the Anterior/Posterior Rectus sheath junction, the posterior rectus sheath was incised to expose the underlying Transversus abdominis muscle. The muscle was then divided along its entire medial edge using electrocautery. This step was initiated in the upper third of the abdomen where medial fibers of the Transversus abdominis muscle are easiest to identify and separate from the underlying fascia.
This step allows entrance to the space between the Transversalis fascia and the divided Transversus abdominis muscle. Below the Arcuate line of Douglas, only Transversalis fascia and peritoneum was medialized. Once a similar release was performed on the other side, the posterior rectus sheaths were re-approximated in the midline with a running monofilament suture. Following this, a suitably sized polypropylene mesh was placed in the preperitoneal space (underlay) and fixed transfascially as laterally as possible. Two drains, one on each side were placed over the mesh. Finally, the linea Alba was recreated by approximating the anterior rectus sheath with a running suture.
Our experience with the above-mentioned procedure enabled us to decide pre-operatively the necessity of CST in these patients, guided by the CSI in these patients as correlated to the operative assessment of defect size. A 1-cm incision was made over the costal margin lateral to the mid-clavicular line [6-8]. A shallow incision was made through the external oblique aponeurosis. A dissecting balloon was used to create space between the external oblique aponeurosis and internal oblique aponeurosis. After the appropriate plane had been dissected through inflation of the balloon, a 12-mm balloon-tipped trocar was placed in the posterior Axillary line between the anterior superior iliac spine and the costal margin under direct vision to help facilitate dissection. The External oblique aponeurosis was divided with hook/sharp scissor cauterization at least 4-cm past the superior and inferior edge of the ventral hernia defect and at least 2 cm lateral to the Semilunar line. After the aponeurosis was divided, the overlying fatty tissue was divided past Scarpa’s fascia to allow further separation of the cut edges of at least 3-4 cm. The external oblique aponeurosis on the contralateral left side was divided in a similar manner. After component separation, in the next step, abdomen was entered laparoscopically and the hernia was reduced. Finally, the medial edges of the rectus were reapproximated in the midline by a continuous running V-loc barbed suture to recreate the linea-alba. Mesh, typically synthetic, composite, was secured [9].
Mesh was fixed with Transfascial sutures at the lower edge and another at the upper edge of the mesh just. Next, the mesh was tacked to the anterior abdominal wall in a double-crown technique with 1 cm gaps.
A MDCT was done and a transverse section showing maximum defect size at full Valsalva maneuver was selected to calculate the Angle of diastasis. The vertex of the angle was taken as the position of the aorta at the axial CT image where the maximal transverse dimension of the hernia defect was identified. The arms of the angle are then taken from this point to the medial edges of the Rectus abdominis muscles. Then the index value was calculated with the Angle of Diastasis (AD) as the numerator and 360 degrees as the denominator. The calculated value served as an accurate biometric assessment of the abdominal wall defect. Postoperatively various parameters were monitored to evaluate outcomes and complications. Follow up was done at 1 week, 1 month and 6 months. All findings were recorded in a preformed proforma.
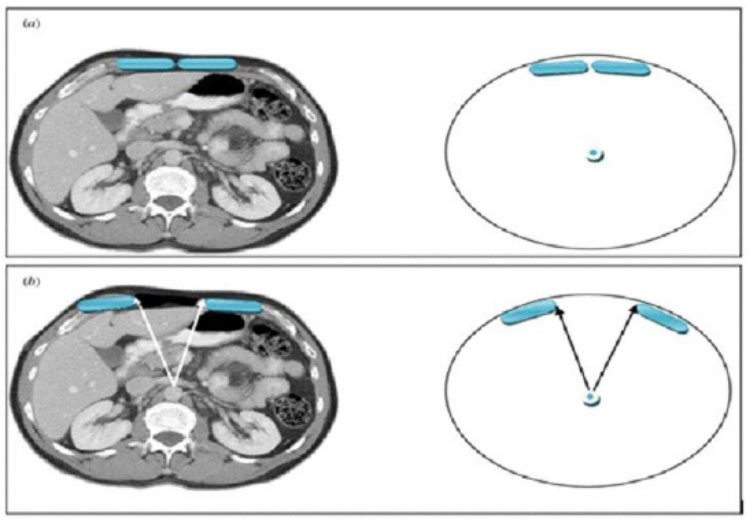 Figure 5: (a): Normal abdominal wall; (b): ventral hernia defect margins denoted by arrowheads forming an
angle of diastasis at a fixed point in the abdomen say, aorta.
Figure 5: (a): Normal abdominal wall; (b): ventral hernia defect margins denoted by arrowheads forming an
angle of diastasis at a fixed point in the abdomen say, aorta.
The observations of the various parameters noted in the study are described below
The age group of patients in our study ranged from 35 years to 80 years for the open group with an average age of 52.8 +/- 13.9 years and 35 years to 65 years for the laparoscopic group with an average age of 52.9 +/- 8.5 years.
In our study, 63% of the patients were female with a predominant female: male ratio of 1.7:1. In the open group, 60% of the patients were female (9/15) whereas in the laparoscopic group 67% of the patients were female (10/15).
Only 24 out of the 90 i.e. 26.7% of patients had a pre-existing co-morbidity. Of these, 15 patients (16.7%) were diabetic and 6 were hypertensive (6.7%) on regular medications. Three patients (3.3%) had both diabetes and hypertension.
Only patients with previous abdominal surgery were included in the study (Incisional hernias). The number of previous surgeries ranged between 1-3 with the average number of previous surgeries being 1.3 for the open group and 1.6 for the laparoscopic group resulting in an overall average of 1.4. Thirty of the ninty patients (33%) had undergone a previous hernia repair and presented with a recurrence.
The mean BMI of patients in our study was 26.3 +/- 5.7 kg/ m2 and included a wide range of underweight patients (BMI=16) to superobese patients (BMI=39.45).
The overall mean defect size in our study was 111.10 cm² with a wide range of defect size (25-486), in the open group the mean defect size was 124.79 cm² and for the laparoscopic group, it was 97.41 cm². The mean angle of diastasis was found to be 34.57° (12-93) resulting in an average component separation index of 0.096 with the minimum CSI for which open component separation needed to be performed being 0.033 setting the cut off value for the laparoscopic group which included patients having CSI ranging from 0.039 to 0.206.
The mean estimated blood loss was 460 +/- 165 ml in the open group and 121 +/- 70 ml in the laparoscopic group. We found the blood loss during surgery to be less with the laparoscopic procedure as compared to open and the result was statistically significant having a p-value (calculated using the unpaired t-test) of <0.05 (Table 1).
| Minimum (ML) | Maximum (ML) | Mean (ML) | SD (ML) | p-value | |
|---|---|---|---|---|---|
| Open | 240 | 800 | 460.67 | +/- 165.21 | 5.704 × 10-8 |
| Lap | 50 | 300 | 121.33 | +/- 70.19 |
We found the mean operative time for an open group (121.8 +/- 34.8 minutes) was lesser as compared to the laparoscopic group (165 +/- 43.2 minutes) presumably related to the steeper learning curve associated with the latter. The difference was of statistical significance with a p-value (calculated using the unpaired t-test) of <0.05 (Table 2).
| Minimum (Minutes) | Maximum (Minutes) | Mean. (Minutes) | SD (Minutes) | p-value | |
|---|---|---|---|---|---|
| Open | 60 | 180 | 121.8 | +/- 34.8 | 0.00628 |
| Lap | 90 | 210 | 165 | +/- 43.2 |
In our study, there were only wound-related complications and no other systemic/mesh-related/iatrogenic complications were observed. Among the wound complications, a haematoma was reported in three of the case (6.7%) of the laparoscopic group while in the open group all wound complications like seroma (46.7%), wound infection (13.3%), skin necrosis (53.3%)and dehiscence (6.7%) were reported. Among the two groups, a statistically significant difference in outcome was reported with respect to seroma formation and skin necrosis, the p-value was calculated using the chi-square test and was < 0.05 with respect to these outcomes (Table 3).
| Seroma | Minimum (Minutes) | Mean. (Minutes) | p-value | ||
|---|---|---|---|---|---|
| Frequency | Percentage | Frequency | Percentage | ||
| 21/45 | 46.70% | 0/45 | 0% | 0.0025 | |
| Wound infection | 6/45 | 13.30% | 0/45 | 0% | 0.1432 |
| Skin necrosis | 24/45 | 53.30% | 0/45 | 0% | 0.00095 |
| Wound dehiscence | 3/45 | 6.70% | 0/45 | 0% | 0.3091 |
| Wound haematoma | 0/45 | 0% | 0/45 | 6.70% | 0.3091 |
| Cough impulse | 0/45 | 0% | 0/45 | 0% | N/a |
| Sinus/fistula | 0/45 | 0% | 0/45 | 0% | N/a |
| Mesh-related complications | 0/45 | 0% | 0/45 | 0% | N/a |
| Mesh removal | 0/45 | 0% | 0/45 | 0% | N/a |
| Enterotomy | 0/45 | 0% | 0/45 | 0% | N/a |
| Illeus | 0/45 | 0% | 0/45 | 0% | N/a |
| Respiratory and cardiac complications | 0/45 | 0% | 0/45 | 0% | N/a |
Patients were mobilised earlier in the laparoscopic group on an average at 1.6 days as compared to a day later for those who underwent the open procedure. The result was interpreted using the unpaired t-test and found to be statistically significant with a p-value of < 0.05
The average length of hospital stay for patients belonging to the laparoscopic group was 5 days +/- 0.9 days as compared to 7.2 days +/- 1.6 days for the open group. The results were interpreted using the unpaired t-test and were statistically significant with a p-value of < 0.05.
Functional outcome in terms of abdominal wall strength like getting up from sitting/squatting position was reported to be better in 80% of the cases. 20% of patients, however, reported no change in the functional outcome. No worse outcome was reported. Among the two groups, the difference in functional outcome was interpreted using the chi-square test and was found to be statistically insignificant with a p-value of 0.0678 (>0.05).
Worse cosmetic outcome was reported in only three cases which were done by open technique and developed skin necrosis, wound infection, and wound dehiscence in the postoperative period. Among the two groups, the difference in cosmetic outcome was interpreted using the chi-square test and was found to be statistically insignificant with a p-value of 0.188 (>0.05).
Morbidity, as reported above, was seen in 33 of the 90 cases i.e, 37%. Wound complications were found in 6.7% of patients of the open group as compared to zero incidences in the laparoscopic group. Chronic pain was reported in 33.3% in the laparoscopic group with zero incidences in the open group, the result interpreted using the chi-square test was of statistical significance, this is stipulated due to the use of transfascial sutures and tackers for fixing of intraperitoneal mesh in the former group which often can result in neuritis. 13.3% of patients in the open group and 20% of patients in the laparoscopic group had complaints of excessive lax skin which was uncomfortable for the patient. At one month no pseudo-recurrence or true recurrence was reported in either of the two groups
Morbidity was seen in 15 of the 90 cases at 6 months follow up i.e. 17%. About 13.3% patients in the laparoscopic group had complaints of chronic pain as compared to zero incidences in the open group presumably resulting from the use of intra-peritoneal mesh which was fixed using transfascial sutures and tackers that might cause neuritis, but this failed to reach statistical significance at 6 months probably due to the small sample size. Skin laxity was reported in 6.7% patients in the open group and 13.4% in the laparoscopic group and the result as interpreted using the chi-square test was of statistical significance (p< 0.05).
Incisional hernias are a common postoperative complication, with an incidence of 5-15% following open abdominal procedures and 1-3% following minimally invasive abdominal procedures. Large abdominal wall defects pose a challenging problem to correct for surgeons. The abdominal wall reconstruction is an evolving field of surgery [10].
In abdominal wall reconstruction for large, complex hernias Component Separation Technique (CST) was developed. Open CST necessitates large subcutaneous skin flaps and, therefore, is associated with significant ischemic wound complications. The Minimally Invasive Or Endoscopic Component Separation Technique (MICST) has been suggested in preliminary studies to reduce wound complication rates post-operatively [10]. We expect the present proposed study will help gather more information regarding the outcome of a component separation technique and supplement the data regarding the same as there has been no such study and data in reference to the Indian population and setup. Worldwide incisional hernias occur in the middle of the elderly age group as it tends to follow an operation for a previous ailment. In a single-institution study conducted by Azoury et al.
[11] in 2014, the age of patients was reported to have a mean of 57 +/- 11 years for the open component separation group and 58 +/- 11 years for the laparoscopic component separation group. In our study, we found that the patients were belonging to a similar age group though with a slightly earlier mean age of presentation of 52.8 +/- 13.9 years for the open group and 52.9 +/- 8.5 years for the laparoscopic group.
The gender demography varies from equal distribution to a skewed one in different parts of the world. In a randomized controlled trial conducted by Lowe et al. [6] in 2000, the sex distribution was 1:1 for the open group and 1.3: 1 for the laparoscopic group. In our study, we found that the sex distribution was 1.5: 1 for the open group (female 60%) and 2:1 for the laparoscopic group (female 67%).
According to a meta-analysis published by Switzer et al. [10] in 2014 which included 7 non-randomized controlled trials conducted outside India, the mean BMI of patients was 31.2 kg/m2 for an open group and 31.3 kg/m² for laparoscopic group. In our study, the mean BMI was reported to be 26.3 kg/m2 with a wide range from 16-39. 53% had a BMI above normal suggesting the link between obesity and incidence of incisional hernias while 7% were malnourished. 17% of the patients were chronic alcoholics while 10% were chronic smokers.
The higher the number of previous surgeries the patient has undergone higher will be the chances of his/her developing an incisional hernia. In our study, we found the average number of previous surgeries to be 1.3 for the open group with 0.3 being the average number of previous hernia repairs and 1.6 for the laparoscopic group with 0.3 being the average number of previous hernia repairs for this group. The study was found to be correlated with a systemic review of 56 case series conducted outside India and published by Switzer et al. [10] in 2014. In the study reported by Lowe et al. [6] in 2000 the mean defect size of hernias for which open component separation was done was 209 cm² (16-988) while for the laparoscopic group it was 288 cm² (170-375). In our study, the overall mean defect size was 111.10 cm2
(25-486), in the open group the mean defect size was 124.79 cm² and for the laparoscopic group, it was 97.41 cm². The mean angle of diastasis was found to be 34.570 (12-93) resulting in an average component separation index of 0.096 with the minimum CSI for which open component separation needed to be performed being 0.033 setting the cut off value for the laparoscopic group which included patients having CSI ranging from 0.039 to 0.206.
Patients having large abdominal wall hernias often have an associated poor pulmonary function owing to the disintegration of the normal dynamic and functional integrity of the abdominal muscles. In our study, 17% of patients had a restrictive pattern of pulmonary function preoperatively and none of them had any post-operative respiratory complaints or complications. According to the study conducted by Agnew et al. [12] in 2010, the component separation repair acts to restore the lost abdominal domain by increasing its volume and can be performed on patients with large ventral hernias with acceptable outcomes and without measurable changes in pulmonary function In the study reported by Lowe et al. [6] in 2000, the estimated average blood loss was 293 ml for the open group and 193 ml for the laparoscopic group. In our study, we found a similar result with significantly less blood loss in the laparoscopic group. In our study, we had found that the operative time to be significantly less as compared to the earlier studies presumably due to better understanding and more data available to us, however the mean operative time for the laparoscopic group was higher (165 min) as compared to the open group (122 min) and the difference was statistically significant which was related to the steeper learning curve with laparoscopy.
We used mesh reinforcement as an advantage of closing the midline in a tensionless fashion following CST is that no meshes are required as was originally proposed by Ramirez et al. However, the present trend is to reinforce the repair by a mesh as it has been found to further reduce recurrences. As only the suture line needs to be protected, a much smaller mesh is required following CST repair. The average mesh: defect ratio was 8.05 (0.45-30).
In the study reported by lowe et al. [6] in 2000 the incidence of midline wound infections, ischemia or skin necrosis, and wound dehiscence was 40, 20 and 43 percent respectively in the open group and had zero incidences in the laparoscopic group. In our study, we found an incidence of 13.3%, 53.3% and 6.7% for wound infection, ischemia and dehiscence in the open group and a zero incidence in the laparoscopic group. The 6 patients who developed wound infection and 3 of them who went onto develop wound dehiscence were known cases of diabetes mellitus and thus predisposed to the above complications. A high percentage of patients had developed blackening of wound margins in the postoperative period in the open group due to surgical damage sustained to the perforating vessels that supply the skin during tissue undermining. A laparoscopic approach avoids the need for these lengthy incisions and extensive dissection and thus preserves the perforating vessels supplying the skin and subcutaneous tissue.
In the study reported by lowe et al. [6], the incidence of ileus, cardiac, renal or respiratory complication in the open group was 27%, 23%, 3%, 23% respectively and for the laparoscopic group, it was 14%, 0%, 0%, 14% respectively. In our study, there were zero incidences of these systemic complications in either group.
The postoperative analgesic requirement was limited to the usage of NSAID’s for the first 2 days and then S.O.S for 90% of the patients. The difference in analgesia requirement for the two groups was statistically insignificant and thus, post-op pain scores can inferentially be thought of as similar for both the procedures.
 Figure 6: (A): Large ventral hernia Pre-perative photo; (B): Post-operative photos and (C): Post-operative photos.
Figure 6: (A): Large ventral hernia Pre-perative photo; (B): Post-operative photos and (C): Post-operative photos.
In the systemic review conducted by Switzer et al. [10], the mean length of hospital stay was reported to be 9.1 and 7.7 days for the open and laparoscopic group respectively. In our study, we found that in the open group patients were discharged after an average hospital stay of 7.2 days whereas for the laparoscopic group this time period was much shorter being 5 days and thus a faster recovery as seen with most laparoscopic surgeries In our study, we took feedback from the patients for functional and cosmetic outcomes. 80% of the patients reported an improved functional outcome in terms of ability to get up from sitting position, 20% of patients who did not report any improvement were found to have long-standing hernias on history. With regards to cosmetic outcome, 90% of patients reported an improved outcome (Figure 6 and 7), 3 patients (3%) who had skin infection in the postoperative period reported the worst outcome while 6 patients (7%) did not report any change in the cosmetic outcome.
In the study by Switzer et al. [10] the open group was followed up for 25.8 months and had a recurrence rate of 11.1% while the laparoscopic group was followed up for 15.5 months and had a recurrence rate of 15.1%. In the study by S.C. Azoury et al. [11] the incidence of recurrence was 0% for the open group and 4% for the laparoscopic group. In our study, with follow up done at 1 month after surgery; wound complication, chronic pain, skin laxity, bulging recurrence had an incidence of 6.7%, 0%, 13.3%, 0%, 0% respectively for the open group and an incidence of 0%, 33.3%, 20%,0%,0% respectively for the laparoscopic group With follow up at 6 months after surgery; wound complication, chronic pain, skin laxity, bulging, recurrence had an incidence of 0%, 0%, 6.7%, 0%, 0% respectively for the open group and 0%, 13.3%, 13.3%, 0%, 0% respectively for the laparoscopic group. The difference in chronic pain between the two groups at 6 months now becomes statistically insignificant as the abdominal wall adapts and tackers get absorbed. The complaint of skin laxity with excess overhanging skin, however, attains statistical significance at 3 months and is reported to be more common with the laparoscopic group which is because the stretched and thinned out skin is not excised as a part of the routine procedure in the laparoscopic group of patients while a part of the lax skin is excised invariably in the open group to allow for optimal scar formation in the new suture line.
 Figure 7: Postoperative photo of a patient who underwent endoscopically assisted laparoscopic component separation technique.
Figure 7: Postoperative photo of a patient who underwent endoscopically assisted laparoscopic component separation technique.
The Component separation done by either a posterior open or endoscopic technique results in good functional and cosmetic outcomes for the patients with no reported recurrences. However, the endoscopic procedure was associated with lesser blood loss and faster recovery
