 Journal of Medical Research and Surgery
PROVIDES A UNIQUE PLATFORM TO PUBLISH ORIGINAL RESEARCH AND REMODEL THE KNOWLEDGE IN THE AREA OF MEDICAL AND SURGERY
Journal of Medical Research and Surgery
PROVIDES A UNIQUE PLATFORM TO PUBLISH ORIGINAL RESEARCH AND REMODEL THE KNOWLEDGE IN THE AREA OF MEDICAL AND SURGERY
 Journal of Medical Research and Surgery
PROVIDES A UNIQUE PLATFORM TO PUBLISH ORIGINAL RESEARCH AND REMODEL THE KNOWLEDGE IN THE AREA OF MEDICAL AND SURGERY
Journal of Medical Research and Surgery
PROVIDES A UNIQUE PLATFORM TO PUBLISH ORIGINAL RESEARCH AND REMODEL THE KNOWLEDGE IN THE AREA OF MEDICAL AND SURGERY
 Indexed Articles
Indexed ArticlesSelect your language of interest to view the total content in your interested language
Ganesh Aher1, Pritesh Kothari2, Yogesh Salphale3 , Gopal Shinde2*
, Gopal Shinde2* , Eknath Pawar
, Eknath Pawar
1Department of Orthopaedics, Jawahar Medical Foundations A.C.P.M. Medical College, and Hospital, Dhule, Maharashtra, India.
2Department of Orthopaedics, Maharashtra Post Graduate Institute of Medical Education and Research, Maharashtra University of Health Sciences, Nashik, Maharashtra, India.
3Shushrusha Multispecialty Hospital, Chandrapur, Maharashtra, India.
4Department of Orthopaedics, Grant Medical College and JJ Hospital, JJ Marg, Byculla, Mumbai, Maharashtra, India.
Correspondence to: Gopal Shinde, Department of Orthopaedics, Maharashtra Post Graduate Institute of Medical Education and Research, Maharashtra University of Health Sciences, Nashik, Maharashtra, India.
Received date: April 04, 2024; Accepted date: April 22, 2024; Published date: April 29, 2024
Citation: Aher G, Kothari P, Salphale Y, et al. Efficacy of Platelet-Rich Plasma Versus Hyaluronic Acid in Symptomatic Knee Osteoarthritis. J Med Res Surg. 2024;5(2):45-51. doi: 10.52916/jmrs244135
Copyright: ©2024 Aher G, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted
use, distribution and reproduction in any medium, provided the original author and source are credited.
Background: Osteoarthritis (OA) is one of the most common forms of arthritis and leading causes of disability. Intra-articular injection of PRP or steroid may provide benefit for patients suffering from osteoarthritis of knees, preventing, and delaying the need of a larger operative measures as many of the senile patients suffering from OA knee are quite hesitant to undergo any operative measure for the same. Materials and Methods: This was prospective type of study, with randomised selection of the patients for the assessment of outcome of treatment of symptomatic knee osteoarthritis with intra articular injections of PRP or hyaluronic acid. This study was carried out in the department of orthopaedics at our institute. In this study both injections given superolaterally weekly for 3 weeks. Study conducted over 2 years, a total of 50 patients suffering from OA knee were included in the study depending upon inclusion criteria. These patients were randomly selected for injection in a sequential manner i.e., case number 1,3,5,7 and so on sequentially were given injection HA. Case number 2,4,6,8 and so on sequentially were given injection PRP. Patients were evaluated prospectively at enrolment and at 6 weeks, 3 and 6-months follow-up with WOMAC and KSS scores. Results: PRP seems to be more efficient as compared to HA in salvaging knee in osteoarthritis. It can work as a salvaging agent in mild to moderate osteoarthritis of knee. HA injection has been found to be effective only in short term cases. Conclusion: The clinical results of this study show that both these non-surgical modalities (intraarticular injections of PRP or HA) are useful for the treatment of osteoarthritis of knee. Treatment with PRP shows significantly better outcome compared with HA group; with respect to WOMAC and KSS scores.
Hyaluronic Acid (HA), Platelet Rich Plasma (PRP) , Osteoarthritis (OA), Knee, Intra-Articular (IA) therapy, Knee Society Score (KSS).
OA is a degenerative and progressive joint disease affects around 250 million people worldwide [1]. Elderly (approximately 35% of patients over 65 years old) females, patients with obesity are the population with the highest risk of developing OA [2,3]. The knee is the largest synovial joint in humans, synovial membrane is in charge of the production of the synovial fluid, which provides lubrication and nutrients to the avascular cartilage [3,4]. Osteoarthritis (OA) knee is a degenerative disorder of multi-factorial aetiology characterized by loss of articular cartilage, hypertrophy of bone at the margins making osteophytes, subchondral sclerosis, and range of some biochemical as well as some morphological alterations of the synovium and joint capsule.
The severity of the disease can also be graded according to the radiographical findings by the Kellgren–Lawrence (KL) system described in 1957. Typical symptoms are pain after prolonged activity and weight bearing; whereas stiffness is experienced after inactivity. Western Ontario and McMaster University Score (WOMAC) for knee and Knee Society Score (KSS) are commonly used scoring system and gives clear idea of effect of disease. Both this scoring system have been used in this study.
Hyaluronic Acid (HA) is a glycosaminoglycan that is naturally present within the synovial fluid of the knee, it provides lubrication to the joint and protects the cartilage from mechanical degradation [5]. HA has been shown to provide anti-inflammatory and chondroprotective effects, increase proteoglycan and HA synthesis, and reduce nerve impulses and nerve sensitivity associated with OA pain [6]. In knee OA, HA is reduced in terms of molecular weight and concentration. Therefore, use of HA is a common and well known Intra-Articular (IA) therapy for knee OA [7]. It inhibits Nitric Oxide (NO) synthesis and may act as free radical scavenger [8,9].
The present study aims to find out the efficacy of intra-articular injections of platelet rich plasma and hyaluronic acid in cases of primary osteoarthritis of knee over 40 years of age and finding out the change in knee function using WOMAC and KSS scores at 6 weeks, 3 and 6 months follow up.
This is prospective study with randomised selection of the patients, the study was carried out in the department of orthopaedics between 2017 to 2019. A total of 50 patients suffering from OA knee were included in the study. These patients were randomly selected for injection in a sequential manner i.e., case number 1,3,5,7 and so on sequentially were given injection HA. In this study both injections given weekly for 3 weeks. Case number 2,4,6,8 and so on sequentially were given injection PRP. Osteoarthritis knee was diagnosed based on history, examination and x-ray findings.
X-ray findings were noted and osteoarthritis was graded using Kellgren-Lawrence grading system as follows: Grade 1: Possible narrowing of joint space and osteophytic lipping. Grade 2: Definite presence of osteophytes and narrowing of joint space. Grade 3: Moderate multiple osteophytes present, definite narrowing of joint space, some form of sclerosis and possible deformity of bone contour. Grade 4: Large osteophytes present, marked narrow joint space, severe sclerosis, and definite deformity of bone contour.
Patients were evaluated prospectively at enrolment and at 6 weeks, 3 and 6-months follow-up with WOMAC and KSS scores according to orthopaedic knee score. Increasing scores shows improvement in functional status.
Collection of blood around 30 to 35 ml through antecubital venepuncture which were divided into 6 to 7 CDPA containing tubes. Then all were subjected to get centrifuged at 3000 rpm for 3 minutes to separate RBCs from plasma at 1st centrifuged cycle (soft spin).
The result of this spin was separation of the whole blood into a lower and upper part, lower red blood cell region and upper straw-coloured plasma. This plasma contains relatively low concentration of platelets (platelet poor plasma) in the uppermost region and higher concentration of platelet in the boundary layer often called as “Buffy Coat.” The tubes were placed in a rack. An equal number of 5 ml tubes without anticoagulant solution were also placed in the rack.
A needle (18 gauge and 78 mm long) was attached to 5 ml syringe to withdraw straw coloured plasma from the tubes by moving the needle from top downward as the draw continues. The draw stopped when an RBC layer was reached or in to the first 1-2 mm of that layer. The straw-coloured plasma was then expressed into the tube without anticoagulant solution. This process was done gently to avoid damage to the platelets. The same procedure was performed with the other tubes.
The tubes with straw coloured plasma were again centrifuged at 4000 rpm for 15 minutes. The tubes were placed in the rack with their cap removed. Now the contents of the tube consist of upper layer of clear supernatant serum containing fibrinogen and very low concentration of platelets. The bottom layer often red tinged consists of highly concentrated platelets.
The upper two third of this liquid was withdrawn and discarded with same spinal needle attached to 5 ml syringe leaving behind one third of the serum with concentrated platelets in the tube. This remaining one third content of the tube was thoroughly mixed to form concentrated platelet rich plasma.
In all the patients in whom PRP was injected, it was injected percutaneously under all aseptic precautions after painting and draping of the part involved. The infiltration technique used for all the groups was the superolateral approach, which has been shown to be the safest, ensuring intra-articular penetration of the drug in up to 93% of cases [10].
The patient was placed in supine position, the medial, lateral, and superior edges of the patella were marked [11], after painting and draping of the part involved, preparation was done from mid-thigh level to mid leg level with the help of povidone iodine solution. A superolateral approach was used whereby the needle was inserted at an angle of approximately 450 towards the medial joint line of the knee until reaching the “soft spot” between the patella and the femur. Before the drug was injected, the piston of the syringe was drawn back slightly to ensure that the needle was properly in the joint.
The mean volume of PRP injected in this study was 3 ml, range was 2-3 ml. At the end of the procedure, the patient was encouraged to bend and extend the knee a few times to allow the PRP to distribute itself all over the joint. Finally, a simple adhesive dressing was done at the injection site. Injection given weekly for 3 weeks.
Post injection the patients were observed for at least half hour. All these injections were given in minor Operation Theatre (OT). HA injection: 2ml IA HA injections were used in this study containing 1% sodium hyaluronic acid which was ready made available. Given weekly for 3 weeks.
Follow Up: Follow up was done at 6 weeks, 3 months, and 6 months. Each time WOMAC and KSS score noted. At each follow up enquiry about symptoms, signs and overall functional improvement in the patient was done.
|
No. of patients studied |
No of patients (50) |
|
PRP Group |
25 |
|
HA Group |
25 |
|
Age Group (years) |
PRP |
HA |
χ2-value |
|
50-54 years |
7(28%) |
2(8%) |
4.44 p-0.349, NS Df-4 |
|
55-59 years |
6(24%) |
10(40%) |
|
|
60-64 years |
5(20%) |
5(20%) |
|
|
65-69 years |
5(20%) |
7(28%) |
|
|
70-74 years |
2(8%) |
1(4%) |
|
|
Total |
25(100%) |
25(100%) |
|
|
Mean ± SD |
60.17±6.31 |
61.04±5.17 |
|
|
Range |
51-71 years |
54-70 years |
With application of unpaired t test on basis of mean and SD values are: t value=0.5333, P-value=0.5963 NS, Df=48. Mean age of the PRP group: around 60 years, range being from: 51-71 years. Mean age of the HA group: around 61 years, range being from: 54-70 years. From above it seems there is no significant difference exist between age in both groups. Majority of the patients were in range of 55 to 69 years, consisting around 38 knees (Table 1-2).
|
Gender |
PRP |
HA |
Total |
χ2-value |
|
Male |
12(48%) |
15(60%) |
27(54%) |
0.725 P value–0.395, NS Df-1.000 |
|
Female |
13(52%) |
10(40%) |
23(46%) |
|
|
Total |
25(100%) |
25(100%) |
50(100%) |
Fishers exact test p-value=0.571, NS. There was total 27 males (12 in PRP group, 15 in HA group) and 23 females (13 in PRP, 10 in HA) amongst total number of patients. So according to this there is no significant association exist between male and females with respect to OA knee (Table 3).
|
Side Involved |
PRP |
HA |
χ2-value |
|
Right |
13 |
13 |
0.000 P value-1.000, NS Df–1 |
|
Left |
12 |
12 |
|
|
Total |
25 |
25 |
Fishers exact test p value- 1.000, NS. Out of the total 50 knees in the study, 26 were right sided and 24 were left sided knees. Statistical value being non-significant based on the side involved, with this results its clearly seen there is no relation exist between side of involvement with OA knee. Equal chances to have OA in both right and left knee (Table 4).
|
|
Mean |
N |
Std. Deviation |
t-value |
p-value |
|
Pre-treatment |
59.61 |
25 |
5.16 |
||
|
6 weeks |
67.61 |
25 |
4.70 |
5.7309 |
0.0001 S |
|
3 months |
72.2 |
25 |
4.84 |
3.4018 |
0.0014 S |
|
6 months |
76.58 |
25 |
4.97 |
3.1568 |
0.0028 S |
Comparison of mean scores at pre-treatment, 6 weeks, 3 and 6 months follow up shows PRP to be significantly effective in improving WOMAC scores and thus proving to be the better choice in long term treatment of OA knee (Table 5).
Above given chart shows sustained improvement in functional status of the patients with respect to WOMAC scores at 6 weeks, 3 and 6 months follow up as compared to pre-treatment value, suggesting effective role of PRP in modifying the progress of disease in OA knee and hence improving the functional outcome of the patients (Figure 1).
|
|
Mean |
N |
Std. Deviation |
t-value |
p-value |
|
Pre-treatment |
58.14 |
25 |
1.4858 |
||
|
6 weeks |
68.32 |
25 |
3.047 |
15.0149 |
0.0001 S |
|
3 months |
69.66 |
25 |
2.7893 |
1.6220 |
0.1114 NS |
|
6 months |
68.61 |
25 |
1.7833 |
1.59 |
0.1183 NS |
In the HA group, mean WOMAC score at 6 weeks (68.32) was higher as compared to baseline value (58.14) at the initiation of treatment, but during later follow ups at 3 months (69.66) and 6 months (68.61) WOMAC scores were found to be not significantly increasing from 6 weeks onwards. This suggested worsening of symptoms and also the functional outcome in the HA group after 6 weeks follow up (Table 6).
Thus, role of HA was found to be short lived lasting only up to 6 weeks as compared to long term action of PRP lasting for at least 6 months (Figure 2).
|
|
PRP Group |
HA Group |
t-value |
p-value |
||
|
|
Mean |
SD |
Mean |
SD |
||
|
Baseline |
59.12 |
5.16 |
58.14 |
1.48 |
0.9128 |
0.3659 NS |
|
6 weeks |
67.61 |
4.70 |
68.32 |
3.047 |
0.6338 |
0.5292 NS |
|
3 months |
72.2 |
4.84 |
69.66 |
2.78 |
2.2753 |
0.0274 S |
|
6 months |
76.58 |
4.97 |
68.61 |
1.78 |
7.5486 |
0.0001 S |
The pre-treatment scores were comparable in both the groups, its clearly seen that there is no significant difference exist before intervention (Table 7).
After application of injection comparison of WOMAC scores in PRP and HA groups shows both the groups to be significantly effective in improving WOMAC scores at 6 weeks follow up there is no significant difference exists between these two modalities of treatments, but at 3 and 6 months follow ups, PRP was found to be more effective as compared to HA in improving functional outcome in patients suffering from OA knee (Figure 3).
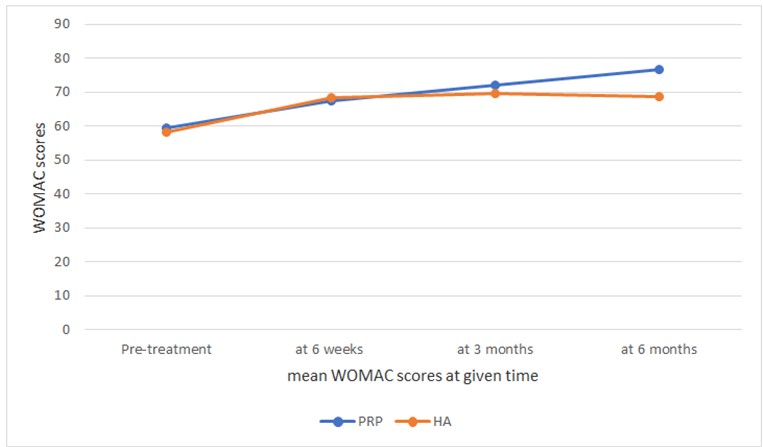 Figure 4: Line diagram showing comparison of mean WOMAC scores in PRP and HA groups at a given time.
Figure 4: Line diagram showing comparison of mean WOMAC scores in PRP and HA groups at a given time.From above line chart its clearly seen PRP has higher mean WOMAC values than HA showing its important role in salvaging OA knee (Figure 4). But at 6 weeks both are equally effective so there is no significant difference exists between them (Table 8).
|
|
Mean |
N |
Std. Deviation |
t-value |
p-value |
|
Pre-treatment |
65.8 |
25 |
1.75 |
||
|
6 weeks |
68.28 |
25 |
1.88 |
4.8278 |
0.0001 S |
|
3 months |
74.72 |
25 |
2.62 |
9.985 |
0.0001 S |
|
6 months |
79.88 |
25 |
2.12 |
7.6551 |
0.0000 S |
Comparison of mean KSS scores at pre-treatment, 6 weeks, 3 months and 6 months follow up shows PRP to be significantly effective in treatment of OA knee. Higher scores were noted subsequently signifying improving functional outcome (Figure 5).
Above given chart shows increase in mean KSS scores at 6 weeks, at 3 months and 6 months follow up as compared to pre-treatment value, suggesting effective role of PRP in modifying the progress of disease in OA knee (Table 9).
|
|
Mean |
N |
Std. Deviation |
t-value |
p-value |
|
Pre-treatment |
64.88 |
25 |
3.01 |
||
|
6 weeks |
67.72 |
25 |
2.85 |
3.4257 |
0.0013 S |
|
3 months |
68.48 |
25 |
3.04 |
0.9119 |
0.3664 NS |
|
6 months |
68.96 |
25 |
2.92 |
-0.5693 |
0.5718 NS |
Above given chart shows increase in mean KSS scores at 6 weeks, at 3 months and 6 months follow up as compared to pre-treatment value, suggesting effective role of PRP in modifying the progress of disease in OA knee (Table 9).
In the HA group, mean KSS score at 6 weeks (67.72) was higher as compared to baseline value (64.88) at the initiation of treatment, but during later follow ups at 3 months (68.48) score slightly improved as compared to previous one and again at 6 months (68.96) KSS scores were found to be slightly increased as compared to previous one. This suggested improving of symptoms in the HA group at 6 weeks but later there is no significant improvement in scores and functional improvement of symptoms as compared to 6 weeks but better than pre-treatment (Figure 6).
|
|
PRP Group |
HA Group |
t-value |
p-value |
||
|
|
Mean |
SD |
Mean |
SD |
||
|
Baseline |
65.8 |
1.75 |
64.88 |
3.01 |
1.3212 |
0.1927 NS |
|
6 weeks |
68.28 |
1.88 |
67.72 |
2.85 |
0.8201 |
0.4162 NS |
|
3 months |
74.72 |
2.62 |
68.48 |
3.04 |
7.7743 |
0.0000 S |
|
6 months |
79.88 |
2.12 |
68.96 |
2.92 |
15.1312 |
0.0000 S |
Thus, role of HA was found to be short lived lasting only up to 6 weeks as compared to long term action of PRP (Table 10).
Comparison of KSS scores in PRP and HA groups showed both the groups to be significantly effective at 6 weeks follow up therefore there is no significant difference exists between two at 6 weeks, but at 3 and 6 months follow ups PRP was found to be more effective in relieving the pain in patients suffering from OA knee. While patients in the HA group showed no significant improvement of mean KSS scores at 3 months and 6 months follow ups (Figure 7,8).
From above line chart its clearly seen PRP has higher mean KSS values than HA showing its important role in salvaging OA knee.
Articular cartilage damage and degeneration in OA are difficult to treat and present a challenge for orthopaedic surgeons, because of the poor blood supply to the hyaline cartilage and its inherent low healing potential. Till date no proven disease modifying therapy is available which can completely halt the process of degeneration. This study is focusing on possibility of preserving normal homeostasis as much as possible or reversing structural damage as a target.
Recently, there is an increase in the use of autologous blood products that might provide cellular and humoral mediators to favour tissue healing in a variety of conditions. The rationale is based on the activity of Growth Factors (GF) carried in blood. The fact that platelets secrete GFs and active metabolites means that their applied use can have a positive influence in clinical situations involving tissues with a low healing potential such as cartilage [12-15].
The clinical results of this study show that both these non-surgical modalities (intra-articular injections of PRP or HA) are useful for the treatment of osteoarthritis of knee. Though HA might have a short-term effect.
Treatment with PRP shows significantly better outcome compared with HA group; with respect to WOMAC and KSS scores which were subsequently improved even at 6 months follow up in the PRP group.
Thus, intra-articular injection of PRP is an efficient treatment modality for salvaging knee in mild to moderate OA.
Despite the relatively low number of patients in each sub-group, statistical analysis confirms better results of PRP than the HA group. Thus, concluding that intra-articular injections of PRP is a more efficient and a better non-surgical treatment modality for treating OA knee when compared to intra-articular injections of HA.
