 Journal of Medical Research and Surgery
PROVIDES A UNIQUE PLATFORM TO PUBLISH ORIGINAL RESEARCH AND REMODEL THE KNOWLEDGE IN THE AREA OF MEDICAL AND SURGERY
Journal of Medical Research and Surgery
PROVIDES A UNIQUE PLATFORM TO PUBLISH ORIGINAL RESEARCH AND REMODEL THE KNOWLEDGE IN THE AREA OF MEDICAL AND SURGERY
 Journal of Medical Research and Surgery
PROVIDES A UNIQUE PLATFORM TO PUBLISH ORIGINAL RESEARCH AND REMODEL THE KNOWLEDGE IN THE AREA OF MEDICAL AND SURGERY
Journal of Medical Research and Surgery
PROVIDES A UNIQUE PLATFORM TO PUBLISH ORIGINAL RESEARCH AND REMODEL THE KNOWLEDGE IN THE AREA OF MEDICAL AND SURGERY
 Indexed Articles
Indexed ArticlesSelect your language of interest to view the total content in your interested language
Abdulrahim Gari1,2* , Samiha Khayyat3, Layan Khushaim4, Roaa Alghamdi5, Wejdan Bagadood6, Sara Bagdood7, Fatimah Alhawsawi8, Fawaz Edris1, Wardah Alasmari9
, Samiha Khayyat3, Layan Khushaim4, Roaa Alghamdi5, Wejdan Bagadood6, Sara Bagdood7, Fatimah Alhawsawi8, Fawaz Edris1, Wardah Alasmari9
1Department of Obstetrics and Gynecology, Faculty of Medicine, Umm Al-Qura University, Makkah, Saudi Arabia
2Department of Obstetrics and Gynecology, King Faisal Specialist Hospital and Research Centre, Jeddah, Saudi Arabia
3King Abdulaziz Medical City, Ministry of National Guard, Jeddah, Saudi Arabia
4General Surgery Resident, King Fahad General Hospital, Jeddah, Saudi Arabia
5General Surgery Resident, King Abdullah Medical Complex, Jeddah, Saudi Arabia
6Family Medicine Resident, Joint Program of Family Medicine in Al Madinah Al Munawarah, Saudi Arabia
7Pediatric Resident, Maternity and Children Hospital, Makkah, Saudi Arabia
8Obstetrics and Gynecology Resident, King Abdulaziz Medical City, Ministry of National Guard, Riyadh, Saudi Arabia
9Department of Anatomy, Faculty of Medicine, Umm Al-Qura University, Makkah, Saudi Arabia
Correspondence to: Abdulrahim Gari, Department of Obstetrics and Gynecology, Faculty of Medicine, Umm Al-Qura University, Makkah, Saudi Arabia.
Department of Obstetrics and Gynecology, King Faisal Specialist Hospital and Research Centre, Jeddah, Saudi Arabia.
Received date: March 07, 2022; Accepted date: March 17, 2022; Published date: March 25, 2022
Citation: Gari A, Khayyat S, Khushaim L, et al. (2022) Awareness of Breast Cancer Screening and Risk Factors among the General Female Population in the Western Province of Saudi Arabia: A Cross-Sectional Study. J Med Res Surg 3(2): pp. 19-30. doi: 10.52916/jmrs224071
Copyright: ©2022 Gari A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License; which permits unrestricted
use; distribution and reproduction in any medium; provided the original author and source are credited.
Background: Worldwide, breast cancer is the most common cancer affecting women, and a common cause of death-related cancer. Fortunately, evidence suggests that we might be able to help improve the outcome with screening, early diagnosis, and intervention.
Objective: The present study investigates the awareness of breast cancer screening and breast cancer risk factors among women in the western province of Saudi Arabia.
Method: The present study employed a cross-sectional survey design, with 365 participating females (aged ≥ 18 years) in the western region of Saudi Arabia. Data were collected from December 2019 to January 2020 using a self-administered questionnaire. The questionnaire covered sociodemographic characteristics, breast cancer knowledge, risk factors, family history, and screening, as well as personal medical history. Data were analyzed using descriptive statistics, chi-square tests, the t-test, and one-way ANOVA tests.
Result: In general, the majority of the women (98.1%) were aware of breast cancer screening. The most commonly identified risk factor in our study was a family history of breast cancer (75.1%), and women with previous exposure to breast cancer measured significantly higher on the socioeconomic index score (M=0.147, SD-0.95) than did those who had never been screened (M=-0.134, SD=1, p=0.007). The findings denote that the women who had a higher knowledge are of a higher socioeconomic class and educational level than were those who were measured and found to have a lower knowledge.
Conclusion: The findings indicate that the level of awareness of breast cancer screening and breast cancer risk factors, including knowledge about mammogram usage, among women of Saudi Arabia is acceptable, being more than a half. However, the results are still sub-optimal and more educational campaigns are needed to improve the knowledge and screening compliance.
Breast cancer, Female population, Risk factor, Hormone Replacement Therapy (HRT), Clinical Breast Examination (CBE), Breast Self-Examination (BSE)
Worldwide, breast cancer is the most common incident cancer and it is the primary cause of cancer-related deaths among women [1]. Approximately 1.7 million women are affected by breast cancer each year, accounting for 23% of all newly diagnosed cancer cases [2]. In 2018, the World Health Organization (WHO) reported that 627,000 women died from breast cancer, representing approximately 15% of all cancerrelated deaths [3].
In 2012, the global cancer project (GLOBOCAN 2012) identified about 1,671,149 new breast cancer cases, and 521,907 deaths due to breast cancer occurred worldwide [4]. Fortunately, one-third of the cases can be successfully treated and lives saved if detected and treated at an early stage [3]. Breast cancer is a disease that develops from breast tissue with different histological subtypes, depending on the cell line origin [2]. Invasive ductal carcinoma, where the cancer cells grow outside the ducts into other parts of the breast tissue, Research and invasive lobular carcinoma, where the cancer cells spread from the lobules to the breast tissues, are considered the most common types of breast cancer. These invasive cancer cells can also metastasize and spread to other parts of the body [5].
Patients may present with different symptoms at different stages. Patients with early stages might be completely asymptomatic. Breast cancer warning signs and symptoms include a new lump in the breast or underarm (Axilla), irritation or dimpling of breast skin, thickening or swelling of part of the breast, redness or flaky skin in the nipple area or the breast, and pain in any area of the breast. These symptoms can also happen with other conditions that are not cancer [6].
Multiple risk factors are associated with the risk of developing breast cancer, and they can be classified into four groups: first, family history and genetic background (accounting for approximately 15% of all breast cancer cases); second, hazardous effects of hormonal exposure, late menopausal age, late age at first birth, a fewer number of children and nulliparity, little or no breastfeeding, and long-term use of Hormone Replacement Therapy (HRT); third, the most significant marker, high breast density; fourth, benign proliferative breast disease history [7]. Additionally, it is commonly believed that stress, poor health behaviors, and toxic environmental exposure could be risk factors for women’s breast cancer [8]. There is marked geographical variation in incidence rates, being highest in the developed world and lowest in the developing countries in Asia, the Middle East, and Africa [9].
Many studies support the idea that regular breast cancer screening can reduce cancer mortality and morbidity by 20– 35%, by facilitating the early diagnosis of cancer [2,10]. The goal of the screening test is to find the disease before any symptoms arise. The breast cancer size and how far it has spread are some of the most important factors in predicting a woman's prognosis (outlook) with this disease [11]. Although breast cancer screening cannot prevent breast cancer, it can help find breast cancer early, when it is easier to treat [12].
Early detection of breast cancer can be achieved through screening mammography, Clinical Breast Examination (CBE), and Breast Self-Examination (BSE) [13]. Poor breast cancer awareness and barriers to accessing healthcare services cause a delay of breast cancer diagnosis in the developing countries [14].
Despite the relatively low incidence of breast cancer in Saudi Arabia compared to other countries, it has been the most common cancer among Saudi females for the past 12 consecutive years (Saudi Cancer Registry, 1994–2005) [15]. In fact, breast cancer is the single leading cause of cancer death for women 20 to 59 years of age, thus posing a major public health concern [16].
In the Middle East and Gulf region, breast cancer incidence is rising and affecting women below the age of 40, compared with Western countries, reaching as high as 20% [15,17]. More than 50% of the cases usually present at an advanced stages (II and III) [7]. Saudi Arabia is one of the Gulf region countries with a Breast Cancer Early Detection Program, which should be applied to all asymptomatic women aged 40-69 year. However, regrettably, there's poor compliance among women to this program. Considering the growth and aging of Saudi Arabia’s population, cancer rates are expected to increase considerably [18]. This will add an enormous burden to the healthcareutilization costs [19]. In this study, we aimed to investigate the awareness of breast cancer screening in women who live in the western province of Saudi Arabia, which may reflect the reason behind the poor compliance.
An obtained consent form was taken by all the participating women before filling out the questionnaire.
A cross-sectional study was performed among the female population in the western province of Saudi Arabia to explore their level of awareness about the risk factors of breast cancer and about mammogram screening. Data were collected from the 1st of December 2019 to the 31st of January 2020. The target population was the female population aged ≥ 18 years, in the western province of Saudi Arabia.
We excluded male gender, female population younger than 18 years, and females who do not live in the western region of Saudi Arabia. The sample size was calculated by an online application (sample size calculator). Data collection was done by a survey based on questionnaires. The Data collection form included 36 questions divided into four sections: socio-demographics, mammogram knowledge, breast cancer knowledge, personal and family history. Sociodemographic information collected included age, nationality, marital status, educational level, monthly income, occupation, and smoking. Twenty-one questions were used to investigate each participant's knowledge about breast cancer risk factors and screening.
Means and standard deviations were used to describe the continuous variables, and categorically measured variables were described with frequency and percentages. The association between categorical variables was measured with the chi-square test and the t-test of independent groups; the one-way ANOVA tests were used to assess the women’s mean knowledge score for statistically significant differences across the levels of binary and multi-level categorical variables, respectively. The Categorical Principal Components Analysis (CATPCA) was used to summarize the measured socioeconomic and educational factors (income, education, employment, and nationality) into one socioeconomic score, to help characterize the combined effect of those educational, economic, and nationality-related factors into the analysis, as a proxy for each woman’s socioeconomic class. The histograms and the Kolmogrove-Smironove tests were used to assess the Normality of continuous variables, and Levene’s test of equal variance was used for the constant variance assumptions.
Multivariate Binary Logistic Regression was used to assess the combined and individual associations between the women's sociodemographic, educational, and past medical conditions. Alongside gynecological factors, the women’s odds of having a high knowledge or previous experience of breast cancer screening were represented in two different models. The associations between those factors, with the women's odds of high knowledge and having breast cancer screening, were expressed as an Odds Ratio as effect size, and the SPSS IBM V.21 was used for the statistical data analysis. The Alpha significance level was considered significant at 0.050 for all the statistical tests we have conducted.
365 women electively enrolled themselves into the study. The descriptive analysis results for their demographic variables are shown in (Table 1), with most of the women (n=182 (49.9%)) aged between 18-30 years. 192 (53.2%) women were married, and the majority (n=286 (78.4%)) were Saudi women, and 79 (21.6%) were expatriates residing in the Kingdom. The women's educational attainment level was an associate diploma or higher for 244 women (66.8%); of those, 165 (45.2%) women had a monthly income between 3,000-10,000 Saudi riyals. Regarding employment, 172 of the women (47.1%) were employed, but 184 (50.4%) were also housewives. Only 33.7% were smokers.
Table 1: Descriptive statistics of women's sociodemographic characteristics (n=365).| Frequency n(%) |
|
|---|---|
| Age group | |
| 18-30 Years | 182 (49.9) |
| 31-40 Years | 80 (21.9) |
| 41-50 Years | 62 (17) |
| 51-60 Years | 27 (7.4) |
| >60 Years | 14 (3.8) |
| Marital state | |
| Married | 192 (53.2) |
| Single | 171 (46.8) |
| Nationality | |
| Saudi | 286 (78.4) |
| Non-Saudi | 79 (21.6) |
| Educational level | |
| High school or less | 121(33.2) |
| Diploma or Higher education | 244 (66.8) |
| Households monthly income (SR) | |
| < 3,000 SR | 132 (36.2) |
| 3,000 – 10,000 SR | 165 (45.2) |
| >10,000 SR | 68 (18.6) |
| Employment | |
| Employed | 172 (47.1) |
| Housewife | 184 (50.4) |
| Retired | 9 (2.5) |
| Actively smoking | |
| No | 242 (66.3) |
| Yes | 123 (33.7) |
| Age started smoking | |
| < 20 Years | 47 (12.9) |
| 21-30 Years | 62 (17) |
| >31 years | 14 (3.8) |
| Not smoker | 242 (66.3) |
| Age < 40 years | 150 (41.1) |
| Painful | 48 (13.2) |
| Never heard of mammogram | 66 (18.1) |
| In your opinion, what is the best method to raise awareness of breast cancer? | |
| Clinics | 68 (18.6) |
| Internet | 20 (5.5) |
| Previous patient cancer | 11 (3) |
| Books | 3 (0.8) |
| Campaigns | 144 (39.5) |
| Media | 119 (32.6) |
Most of the women in the sample (n=307 (84.1%)) were in their pre-menopause age. Only 12 (3.3%) of them had been diagnosed with breast cancer previously. Nonetheless, 112 (30.7%) of the women had a positive family history of breast cancer, and 31 (8.5%) had recently been diagnosed with benign breast disease
Interestingly, almost half of the respondent women (n=174 (47.7%)) advised that they had previously been screened for breast cancer, as shown in (Table 2).
Table 2: Descriptive statistics for women's medical and gynecological history and breast cancer screening practices (n=365).| Frequency n(%) | |
|---|---|
| Do you still get your regular menstrual period | |
| no | 58 (15.9) |
| yes | 307 (84.1) |
| When do you expect your menstrual cycle to cease | |
| Already in menopause | 58 (15.9) |
| 40-50 years | 120 (32.9) |
| >50 years | 187 (51.2) |
| Have you been diagnosed with breast cancer? | |
| no | 353 (96.7) |
| yes | 12 (3.3) |
| Has your family member been diagnosed with breast cancer? | |
| no | 253 (69.3) |
| yes | 112 (30.7) |
| Have you been diagnosed with or currently have a benign breast tumor? | |
| No | 334 (91.5) |
| Yes | 31 (8.5) |
| Have you or your family member been diagnosed with a benign breast tumor? | |
| No | 258 (70.7 |
| yes | 107 (29.3) |
| Have you ever had a breast cancer screening? | |
| No | 191 (52.3) |
| Yes | 174 (47.7) |
| If screened, how did you screen? | |
| Never been screened | 191 (52.3) |
| Breast self-examination | 120 (32.9) |
| Manual examination by the doctor | 17 (4.7) |
| Ultrasound (US) | 8 (2.2) |
| Mammogram | 26 (7.1) |
| MRI | 3 (0.8) |
| Why do you think women avoid mammograms | |
| Unsure | 55 (15.1) |
| Cannot afford cost | 46 (12.6) |
| Doctor | 74 (20.3) |
| Family or Friends | 63 (17.3) |
| Social Media | 101 (27.7) |
| TV Or Radio | 14 (3.8) |
| Books | 21 (5.8) |
| Do you think breast cancer is widely spread? | |
| No | 61 (16.7) |
| Yes | 304 (83.3) |
| In your opinion, at what age should a mammogram be started? | |
| < 40 years | 126 (34.5) |
| 41 -50 years | 108 (29.6) |
| >50 Years | 37 (10.1) |
| Do not know | 94 (25.8) |
| In your opinion, how often a mammogram must be done? | |
| Every 6 months | 72 (19.7) |
| Every year | 107 (29.3) |
| Every 2 years | 59 (16.2) |
| Do not know | 127 (34.8) |
| Do you think, regular screening should be done by? | |
| Family doctor | 56 (15.3) |
| Surgeon | 58 (15.9) |
| Do not know | 63 (17.3) |
The majority of women (n=358 (98.1%)) were aware of breast cancer screening as a general idea, and 273 (74.8%) women advised that they had previously heard about the mammogram as a screening method; however, 304 women (83.3%) believed that breast cancer is common in the society.
Only 37 (10.1%) of the women knew that routine mammogram screening should start after the age of fifty years, but, also surprisingly, another 94 (25.8%) women advised that they did not know what it is. Upon asking about the right frequency of breast cancer screening with a mammogram, only 59 (16.2%) women had correctly selected screening every two years, but, unfortunately, 127 (34.8%) women answered with "Do Not Know," as shown in (Table 3A).
| Frequency n(% | |
|---|---|
| Have you Ever heard of Breast Cancer screening | |
| No | 7 (1.9) |
| Yes | 358 (98.1) |
| Have you Ever heard of mammogram | |
| No | 92 (25.2) |
| Yes | 273 (74.8) |
| Where did you hear the mammogram? | |
| Never heard of it | 92 (25.2) |
The most commonly identified risk factors were a family history of breast cancer (75.1%), followed by personal history (74.2%). A history of chest radiation and smoking were also identified as risk factors by more than half the participants (73.2% for both). Early menstrual periods and early marriage were the two leastidentified risk factors (20.0% and 10.4%, respectively). Most women had inferred that healthy food and breastfeeding are preventive measures against breast cancer (81.1% and 75.6%, respectively), as shown in (Table 3B).
Table 3B: Descriptive Analysis of the women's knowledge on breast cancer risk factors (n=365).| Incorrect n(%) | Correct n(%) | p-value | |
|---|---|---|---|
| Multiparity | 211 (57.8%) | 154 (42.2) | < 0.001 |
| History of previous breast cancer | 94 (25.8) | 271 (74.2) | < 0.001 |
| Exposure to radiation | 98 (26.8) | 365 (73.2) | < 0.001 |
| Late menstrual period | 230 (63) | 135 (37) | < 0.001 |
| Early menstrual period | 292 (80) | 73 (20) | < 0.001 |
| Alcohol consumption | 136 (37.3) | 229 (62.7) | < 0.001 |
| Use of contraceptives | 173 (47.4) | 192 (52.6) | 0.32 |
| Obesity | 156 (42.7) | 209 (57.3) | 0.006 |
| Early marriage | 327 (89.6) | 38 (10.4) | < 0.001 |
| Breast feeding | 89 (24.4) | 276 (75.6) | < 0.001 |
| Hormones treatment | 163 (44.7) | 202 (55.3) | 0.041 |
| Family history of breast cancer | 91 (24.9) | 274 (75.1) | < 0.001 |
| History of previous ovarian cancer | 151 (41.4) | 214 (58.6) | 0.001 |
| Family history of ovarian cancer | 145 (39.7) | 220 (60.3) | < 0.001 |
| Healthy food | 69 (18.9) | 296 (81.1) | < 0.001 |
| Smoking | 98 (26.8) | 267 (73.2) | < 0.001 |
| Older age | 190 (52.1) | 175 (47.9) | 0.432 |
Overall knowledge on breast cancer risk and screening was computed via rewarding each correctly answered question (of the 21 knowledge questions) with two points, and zero was awarded for incorrectly answered questions. The resulting descriptive analysis in (Table 4) shows that the women had an overall mean knowledge score of 46.31 out of 100, SD=24.3.
Table 4: Descriptive statistics for the women overall knowledge on breast Screening in (%).| Mean (SD) | 46.31 (24.3) | |
|---|---|---|
| Minimum | 0 | |
| Maximum | 80.95 | |
| Percentiles | 25th |
33.33 |
| 50th | 52.38 | |
| 75th | 61.9 | |
According to an independent groups t-test, the women who were older than 40 years tended to have lower knowledge on breast cancer screening and risk, on average (p=0.026), as shown in (Figure 1). However, educated women with a diploma or higher measured slightly higher on the knowledge score (p=0.059).
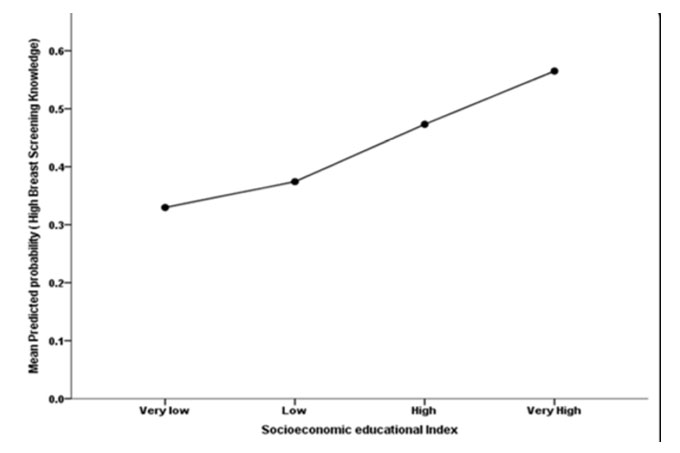 Figure 1: The association between womens Mean Breast cancer risk screening knowledge (%) and their age groups.
Figure 1: The association between womens Mean Breast cancer risk screening knowledge (%) and their age groups.
On the other hand, those women with a monthly household income above 10,000 SAR measured significantly higher in knowledge about screening (p>0.001), as did employed women, than did those who are housewives (p=0.005), as shown in (Table 5A and 5B).
Table 5A: Bivariate analysis of the women's mean breast cancer risk screening knowledge across their sociodemographic characteristics (n=365).| Breast Screening Knowledge Mean (SD | Test statistic |
p-value | |
|---|---|---|---|
| Age group | |||
| 18-30 Years | 47.91 (19.8) | f(4,360)=1.52 | 0.197 |
| 31-40 Years | 47.97 (22.1) | ||
| 41-50 Years | 40.86 (21.7) | ||
| 51-60 Years | 44.80 (22.9) | ||
| >60 Years | 43.20 (27.7 | ||
| Age groups collapsed | |||
| < 40 Years | 47.93 (20.50) | t(170.76)=2.33 | 0.026 |
| > 41 Years | 42.21 (22.72) | ||
| Marital state | |||
| Married | 46.02 (21.7) | t(363)=0.30 | 0.781 |
| Single | 46.64 (20.8) | ||
| Nationality | |||
| Saudi | 47.25 (20.9) | t(363)=1.61 | 0.109 |
| Non-Saudi | 42.92 (22.2) | ||
| Educational level | |||
| High school or less | 43.33 (21.8) | t(363)=1.90 | 0.059 |
| Diploma or Higher education | 47.80 (20.9) |
||
| Households monthly income (SR) | |||
| < 3,000 SR | 41.27 (21.7) | f(2,362)=9.21 | < 0.0013 |
| 3,000-10,000 SR | 46.98 (20.6) | ||
| >10,000 SR | 54.48 (19.3) | ||
| Employment | |||
| Employed | 49.89 (19.6) | f(2,362)=5.10 | 0.007 |
| Housewife | 42.83 (22.3) | ||
| Retired | 49.21 (20.6) | ||
| Actively smoking | |||
| No | 44.41 (22.1) | t(279.9)=2.53 | 0.012 |
| Yes | 50.06 (19.0) | ||
| Age started smoking | |||
| None-smoker | 44.41 (22.1) | f(3,52.20)=1.83 Welch | 0.048 |
| < 20 Years | 49.54 (18.9) | ||
| 21-30 Years | 49.00 (19.4) | ||
| 31-40 Years | 53.97 (18.0) | ||
| >41 Years | 57.14 (18.8) | ||
| Breast Screening Knowledge Mean (SD) |
Test statistic | p-value |
|
|---|---|---|---|
| Do you still get your regular menstrual period | |||
| No | 42.53 (23.1) | t(363)=1.50 | 0.139 |
| Yes | 47.03 (20.9) | ||
| When do you expect your menstrual cycle to cease | |||
| < 40 | 49.40 (20.78) | f(2,304)=3.29 | 0.0740 |
| 40-50 Years | 43.89 (21.9) | ||
| >50 Years | 49.05 (19.9) | ||
| Have you been diagnosed with breast cancer? | |||
| No | 46.66 (21.2) | t(363)=1.70 | 0.091 |
| Yes | 36.11 (21.2) | ||
| Has your family member been diagnosed with breast cancer? | |||
| No | 45.21 (22.4) | t(256.6)=1.62 | 0.108 |
| Yes | 48.81 (18.3) | ||
| Have you been diagnosed with or currently have a benign breast tumor? | |||
| No | 46.56 (21.1) | t(363)=0.74 | 0.462 |
| Yes | 43.63 (23.5) | ||
| Have you or your family member been diagnosed with a benign breast tumor? | |||
| No | 44.56 (22.2) | t(240.3)=2.50 | 0.008 |
| Yes | 50.56 (18.2) | ||
| Have you ever had a breast cancer screening? | |||
| No | 43.26 (22.5) | t(362)=2.93 | 0.004 |
| Yes | 49.67 (19.4) | ||
| If screened, how did you screen? | |||
| Never been screened | 43.26 (22.5) | f(5,7.83)=2.641 Brown-Forsythe x | 0.109 |
| Breast self-examination | 51.75 (19.2) | ||
| Manual examination by the doctor | 38.66 (18.7) | ||
| Ultrasound (US) | 49.40 (10.8) | ||
| Mammogram | 48.72 (19.2) | ||
| MRI | 38.10 (35.9) | ||
| Why do you think women avoid mammograms | |||
| Cannot afford cost | 46.79 (19.5) |
f(3,113.9)=7.9 | < 0.001 |
| Age < 40 years | 50.38 (19.1) | ||
| Painful | 50.50 (21.5) | ||
| Never heard of mammogram | 34.34 (24.1) | ||
| In your opinion, what is the best method to raise awareness of breast cancer? | |||
| Clinics | 42.23 (20.5) |
f(5,359)=1.60 | 0.159 |
| Internet | 43.33 (22.6) | ||
| Previous patient cancer | 46.75 (22.0) | ||
| Books | 46.03 (16.7) | ||
| Campaigns | 45.17 (21.7) | ||
| Media | 50.50 (20.7) | ||
| Have you ever heard of breast cancer screening | |||
| No | 34.69 (26.6) | t(363)=1.50 | 0.145 |
| Yes | 46.54 (21.1) | ||
| Have you ever heard of mammogram? | |||
| No | 36.90 (22.9) | t(139.4)=4.71 | < 0.001 |
| Yes | 49.49 (19.7) | ||
| Where did you hear the mammogram? | |||
| Doctor | 50.84 (17.2) |
f(4,58.96)=2.70 | 0.039 |
| Family Or Friends | 50.79 (16.4) | ||
| Social media | 45.73 (21.4) | ||
| TV Or Radio | 46.26 (25.8) | ||
| Books | 61.22 (20.1) | ||
Women who learned from social media measured significantly lower in knowledge as compared to those learning from books, on average (p=0.029). Interestingly, the analysis model showed that women's Socioeconomic Class Score (SES) converged positively and significantly on greater odds of having a high breast cancer risk factors knowledge (O.R=1.24 times more), on average, above and over the effect of their educational level and nationality (p=0.002), as shown in (Table 5C) and in (Figure 2).
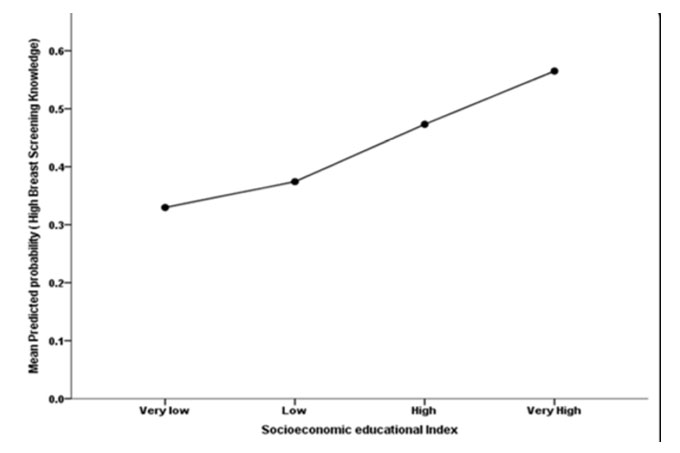 Figure 2: The association between women’s socioeconomics index and their adjusted probability of having had high breast cancer screening knowledge.
Figure 2: The association between women’s socioeconomics index and their adjusted probability of having had high breast cancer screening knowledge.
| B | S.E. | Wald | Adjusted Odds Ratio |
95% C.I. for O.R |
p-value | ||
|---|---|---|---|---|---|---|---|
| Lower | Upper | ||||||
| Age group > 41 years | -0.138 | 0.228 | 0.37 | 0.871 | 0.557 | 1.36 | 0.543 |
| Nationality=Saudi | -0.388 | 0.342 | 1.284 | 0.678 | 0.347 | 1.327 | 0.257 |
| Marital state= Married | 0.075 | 0.234 | 0.102 | 1.078 | 0.681 | 1.705 | 0.749 |
| Educational level >High school | -0.619 | 0.37 | 2.799 | 0.538 | 0.261 | 1.112 | 0.094 |
| Socioeconomic class score/Index | 0.598 | 0.197 | 9.2 | 1.818 | 1.236 | 2.676 | 0.002 |
| Smoker=Yes | 0.27 | 0.234 | 1.331 | 1.311 | 0.828 | 2.075 | 0.249 |
| Diagnosed with breast cancer=Yes | -2.12 | 1.066 | 3.959 | 0.12 | 0.015 | 0.969 | 0.047 |
| Previously educated/heard of Mammogram=Yes |
0.814 | 0.276 | 8.683 | 2.257 | 1.313 | 3.879 | 0.003 |
| Constant | -0.029 | -0.556 | 0.003 | 0.971 | 0.958 | ||
| Dependent Variable= High/Low Breast cancer screening knowledge; Model Hosmer-Lemeshow Goodness of Fit statistic; χ2 (8)=9.8; p=0.282; Model AUC ROC=0.70 | |||||||
Moreover, the chi-square test of association suggests that married women and women with incomes above 3,000 SAR are significantly more likely to be screened than others (p=0.028, p=0.006, respectively). Likewise, housewives were found to be significantly less likely to be screened, as compared to employed and retired women (p=0.048). The statistical analysis findings show that neither a woman's nationality nor her educational level was correlated significantly with previous screening (p>0.050).
Interestingly, women with previous exposure to breast cancer measured significantly higher on the socioeconomic index score (M=0.147, SD-0.95) than did those who had never been screened (M=-0.134, SD=1, p=0.007), as shown in (Table 6A). Women with a positive family history of breast cancer were significantly screened more than were those with a negative family history of breast cancer (p=0.001).
Table 6A: Bivariate analysis of the women's previous breast screening exposure across the levels of their sociodemographic characteristics (n=365).| Previously Breast Screened n(%) | ||||
|---|---|---|---|---|
| No | Yes | Test statistic | p-value |
|
| Age group | ||||
| 18-30 Years | 100 (52.4) | 82 (47.1) |
χ2 (4)=1.60 | 0.812 |
| 31-40 Years | 40 (20.9) | 40 (23) | ||
| 41-50 Years | 29 (15.2) | 33 (19) | ||
| 51-60 Years | 15 (7.9) | 12 (6.9) | ||
| >60 Years | 7 (3.7) | 7 (4) | ||
| Marital state | ||||
| Single | 101 (52.9) | 72 (41.4) | χ2 (1)=4.83 | 0.028 |
| Married | 90 (47.1) | 102 (58.6) | ||
| Nationality | ||||
| Saudi | 144 (75.4) | 142 (81.6) | χ2 (1)=2.10 | 0.15 |
| Non-Saudi | 47 (24.6) | 32 (18.4) | ||
| Educational level | ||||
| High school or less | 67 (35.1) | 54 (31) | χ2 (1)=0.67 | 0.412 |
| Diploma or Higher education | 124 (64.9) | 120 (69) | ||
| Households monthly income (SR) | ||||
| < 3,000 SR | 83 (43.5) | 49 (28.2) | χ2 (2)=10.30 | 0.006 |
| 3,000-10,000 SR | 80 (41.9) | 85 (48.9) | ||
| >10,000 SR | 28 (14.7) | 40 (23) | ||
| Employment | ||||
| Employed | 79 (41.4) | 93 (53.4) | χ2 (2)=6.05 | 0.048 |
| Housewife | 108 (56.5) | 76 (43.7) | LR | |
| Retired | 4 (2.1) | 5 (2.9) | ||
| Socioeconomic score, mean (SD) | -0.134 (1) | 0.147 (0.95) | t(363)=2.7 | 0.007 |
| Actively smoking | ||||
| No | 142 (74.3) | 100 (57.5) | χ2 (1)=11.6 | 0.001 |
| Yes | 49 (25.7) | 74 (42.5) | ||
| Age started smoking, n=123 | ||||
| < 20 Years | 23 (46.9) | 24 (32.4) | χ2 (2)=2.90 |
0.24 |
| 21-30 Years | 22 (44.9) | 40 (54.1) | ||
| >31 Years | 4 (8.2) | 10 (13.5) | ||
Interestingly, women who advised they have never heard about the mammogram were significantly less previously screened (p=0.044), according to the chi-square test. In contrast, women who had previously been educated on mammograms weresignificantly more exposed to previous screening (p< 0.001).
Although women's previously accessed sources of information on mammograms did not correlate significantly with their past screening (p=0.071), those who were educated by their doctors were slightly more likely to have had a previous mammogram screening, as shown in (Table 6B).
Table 6B: Bivariate analysis of the women's previous breast screening exposure across the levels of their past medical and gynecological history characteristics (n=365).| Previously Breast Screened n(%) | ||||
|---|---|---|---|---|
| No=191 | Yes=174 | Test statistic | p-value | |
| Do you still get your regular menstrual period | ||||
| No | 27 (14.1) | 31 (17.8) | χ2 (1)=0.92 | 0.337 |
| Yes | 164 (85.9) | 143 (82.2) | ||
| When do you expect your menstrual cycle to cease | ||||
| <40 Years | 7 (4.3) | 4 (2.8) | χ2 (2)=6.30 | 0.067 |
| 40-50 Years | 74 (40.9) | 46 (29.4) | ||
| >50 Years | 90 (54.9) | 97 (67.8) | ||
| Have you been diagnosed with breast cancer? | ||||
| No | 188 (98.4) | 165 (94.8) | χ2 (1)=3.72 | 0.054 |
| Yes | 3 (1.6) | 9 (5.2) | ||
| Has your family member been diagnosed with breast cancer? | ||||
| No | 147 (77) | 106 (60.9) | χ2 (1)=11.02 | 0.001 |
| Yes | 44 (23) | 68 (39.1) | ||
| Have you been diagnosed with or currently have a benign breast tumor? | ||||
| No | 148 (96.3) | 150 (86.2) | χ2 (1)=12.02 | 0.001 |
| Yes | 7 (3.7) | 24 (13.8) | ||
| Have you or your family member been diagnosed with a benign breast tumor? | ||||
| No | 157 (82.2) | 101 (58) | χ2 (1)=25.6 | < 0.001 |
| Yes | 34 (17.8) | 73 (42) | ||
| Why do you think women avoid mammograms | ||||
| Cannot afford cost | 23 (12.6) | 23 (18.1) | χ2 (3)=8.1 | 0.044 |
| Age < 40 years | 82 (44.8) | 68 (53.5) | ||
| Painful | 30 (16.4) | 18 (14.2) | ||
| Never heard of mammogram | 48 (26.2) | 18 (14.2) | ||
| In your opinion, what is the best method to raise awareness of breast cancer? | ||||
| Clinics | 25 (13.1) | 43 (24.7) | χ2 (5)=12.3 | 0.031 |
| Internet | 10 (5.2) | 10 (5.7) | ||
| Previous patient with cancer | 7 (3.7) | 4 (2.3) | ||
| Books | 2 (1) | 1 (0.6) | ||
| Campaigns | 88 (46.1) | 58 (32.2) | ||
| Media | 59 (30.9) | 60 (34.5) | ||
| Have you ever heard of breast cancer screening? | ||||
| No | 7 (3.7) | 0 | χ2 (1)=4.70 | 0.03 |
| Yes | 184 (96.3) | 174 (100) | ||
| Have you ever heard of mammogram? | ||||
| No | 69 (36.1) | 23 (13.2) | χ2 (1)=25.3 | < 0.001 |
| Yes | 122 (63.9) | 151 (86.8) | ||
| Where did you hear the mammogram? n=273 | ||||
| Doctor | 23 (18.7) | 51 (34) | χ2 (4)=8.63 | 0.071 |
| Family or Friends | 31 (25.2) | 32 (21.3) | ||
| Social Media | 52 (42.3) | 49 (32.7) | ||
| TV Or Radio | 6 (4.9) | 8 (5.3) | ||
| Books | 11 (8.9) | 10 (6.7) |
||
Finally, the analysis model, (Table 6C), indicates that women's knowledge of breast cancer screening did not correlate significantly with their odds of having had a previous screening (p=0.122), when accounting for the other factors in the analysis model.
Table 6C: Multivariate binary logistic regression analysis of the women odds of having had previous breast screening (n=365).| B | S.E. | Wald | Adjusted Odds Ratio |
95% C.I. for O.R
|
p-value | ||
|---|---|---|---|---|---|---|---|
| Lower | Upper | ||||||
| Age >40 years | -0.241 | 0.317 | 0.577 | 0.786 | 0.422 | 1.463 | 0.448 |
| Nationality=Saudi National | -0.277 | 0.385 | 0.517 | 0.758 | 0.357 | 1.612 | 0.472 |
| Marital state=Married | 0.549 | 0.269 | 4.183 | 1.732 | 1.023 | 2.933 | 0.041 |
| Educational level > Diploma level | -0.825 | 0.437 | 3.566 | 0.438 | 0.186 | 1.032 | 0.059 |
| Socioeconomic class index | 0.495 | 0.227 | 4.742 | 1.64 | 1.051 | 2.559 | 0.029 |
| Currently smoker=Yes | 0.795 | 0.272 | 8.519 | 2.215 | 1.298 | 3.777 | 0.004 |
| Positive family history of Benign tumor=Yes | 1.338 | 0.293 | 20.897 | 3.81 | 2.147 | 6.761 | < 0.001 |
| Perceived reason for avoiding Mammograms | -0.658 | 0.135 | 23.837 | 0.518 | 0.398 | 0.674 | < 0.001 |
| Previously informed on mammogram=Yes | 0.599 | 0.391 | 2.348 | 1.821 | 0.846 | 3.919 | 0.125 |
| Knowledge score (%) on breast cancer risk screening |
0.01 | 0.007 | 2.397 | 1.01 | 0.997 | 1.023 | 0.122 |
| Constant | 0.105 | 0.719 | 0.021 | 1.11 | 0.884 | ||
| Dependent Variable=Past experience of breast cancer screening Yes/No; Model Hosmer-Lemeshow Goodness of Fit statistic; χ2 (8)=9.72; p=0.285; Model AUC ROC=0.80 | |||||||
Breast cancer is the most common cancer among females worldwide [3]; fortunately, early detection by mammogram screening may contribute to decreasing the disease mortality and morbidity [20]. Saudi Arabia is one of the countries with a Breast Cancer Early Detection Screening Program, which is applied in most hospitals in all regions of Saudi Arabia among females aged 40 to 69 who show no symptoms of breast cancer [18]. In the present study, we investigated the awareness of breast cancer screening, risk factors, and factors that affect this knowledge among the general female population in the western province of Saudi Arabia.
We found that most participants (98.1%) had heard about breast cancer screening from social media, which became the most common source of information. This finding was consistent with a study conducted by Rahman et al. [21], among female students at the University of Sharjah in the United Arab Emirates (UAE). It showed that social media was the main source of information on breast cancer screening ( 98.8%) [21]. Similarly, a study in Egypt by Boulos et al. [22] among female students showed that the main source of information was the mass media (TV and radio) in 89.1% of the participants [22]. Another study in Yemen also reported mass media as the main source of information for 81.6% of participants [23]. The studies in the UAE, Egypt, and Yemen among university students may reflect the impact of technology penetration. In general, our sample was a group of women from the general population who lived in the western province of Saudi Arabia in 2020, reflecting the impact of technology—not the education level—in the general population. On the other hand, however, the level of awareness affected by the educational level was for diploma only, whereas higher education had a higher level of awareness by 47.8% of the participants, which is consistent with previous studies [2426]. Mahfouz et al. reported in a study conducted in Abha city, southwestern Saudi Arabia (2013), that only 22% of participants had heard about a mammogram [27]. In the present study, we found that 74.8% of participants knew that the mammogram is the screening modality for breast cancer, but only 10.1% were aware that it starts at the age of 50, and 16.2% knew it should be repeated every two years in an average-risk female. In a recent study in Syria by Omar et al. among females at Syrian Private University [2], they reported 71% of participants were aware of mammograms as a modality of breast cancer screening [2]. The difference in the reported awareness between our study and the study conducted in Abha is probably related to the time difference, as that was back in 2013 (almost six years before our study) and the increased awareness may reflect the impact of the social media and educational campaign in improving awareness over time among women.
Although women aged older than forty years have lower breast cancer screening and knowledge about the risk factors, only 41.8% of the study population had heard about the mammogram. On the other hand, the most common cause of not having a mammogram done in the past is that they didn't hear about it, followed by thinking it might be painful. This concern was consistent with the reported findings of a study conducted by Boulos et al. in Egypt [22]. More than half of the participants knew that older age, family, or a personal history of breast cancer, late menopause, and early menarche are known risk factors for breast cancer. They were also aware that multiparities, breastfeeding, early marriage, and a healthy lifestyle are protective factors. Knowing it was more than 50% is probably acceptable, but we could not find other studies assessing awareness of breast cancer risk factors. Our study shows that 57.3% of participants were aware that obesity is considered a risk factor for breast cancer, which is similar to the results of another study conducted in Syria by Omar et al., of which 51% of participants did know that [2]. In a study conducted among female university students in Angola, Sambanje et al. [28] also reported a similar finding, that 57% were aware that obesity is a risk factor.
We found that, among the participants, only 12 patients had a personal history of breast cancer (6.8%), while the others never had a history of breast cancer (93.2%). Among the affected cases, only nine patients had had a screening mammogram done prior to the diagnosis (2.5%). As expected, a family history of breast cancer was associated with a significantly higher screening rate in our study population, 23% vs 39.1% (p< 0.001). A similar higher screening rate was reported in patients with a personal history of benign breast disease, 3.7% vs 13.8% (p< 0.001). We did not find in the literature a comparison study to assess the impact of breast cancer on screening compliance; however, Sambanje et al. [28] reported that, in those with a family history of benign diseases, no previous screening was found in 96.3%. This low screening rate corresponded to our findings in this study, in which (82.8%) of the patients with a family history of benign breast disease never had a screening mammogram.
In general, the level of women's awareness of breast cancer screening and of the mammogram, as well as of breast cancer risk factors, is still suboptimal and reaches around half the female population in the area. Low awareness may also reflect low compliance. There is a need for greater support of healthcare providers and for educational/social media campaigns to improve public awareness, acceptability, and compliance, all of which may impact the early detection and hence the treatment of breast cancer and its prognosis. Further studies are needed to investigate the accessibility and obstacles in the system to improve awareness and compliance, which will enhance the screening program in Saudi Arabia.
The authors report no conflict of interest.
No funding or grant support.
