 Journal of Medical Research and Surgery
PROVIDES A UNIQUE PLATFORM TO PUBLISH ORIGINAL RESEARCH AND REMODEL THE KNOWLEDGE IN THE AREA OF MEDICAL AND SURGERY
Journal of Medical Research and Surgery
PROVIDES A UNIQUE PLATFORM TO PUBLISH ORIGINAL RESEARCH AND REMODEL THE KNOWLEDGE IN THE AREA OF MEDICAL AND SURGERY
 Journal of Medical Research and Surgery
PROVIDES A UNIQUE PLATFORM TO PUBLISH ORIGINAL RESEARCH AND REMODEL THE KNOWLEDGE IN THE AREA OF MEDICAL AND SURGERY
Journal of Medical Research and Surgery
PROVIDES A UNIQUE PLATFORM TO PUBLISH ORIGINAL RESEARCH AND REMODEL THE KNOWLEDGE IN THE AREA OF MEDICAL AND SURGERY
 Indexed Articles
Indexed ArticlesSelect your language of interest to view the total content in your interested language
Yulia Bogdanova Peeva*
Department of Social Medicine and Public Health, Faculty of Public Health, Medical University, Plovdiv, Bulgaria.
Correspondence to: Yulia Bogdanova Peeva, Department of Social Medicine and Public Health, Faculty of Public Health, Medical University, Plovdiv, Bulgaria.
Received date: September 4, 2024; Accepted date: September 18, 2024; Published date: September 25, 2024
Citation: Peeva YB. Avulsed 11, Reimplantation, Subsequent Orthodontic Treatment: A Case Report and Literature Review of Child with Epilepsy. J Med Res Surg. 2024;5(5):116-120. doi: 10.52916/jmrs244149
Copyright: ©2024 Peeva YB. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Background: A case report of avulsion of a right central incisor in 9-year-old child is presented. Avulsion is a serious dental injury that requires emergency treatment. Timely and correct emergency care is of particular importance for the prognosis. In this case, it refers to a permanent tooth completely knocked out of the alveolus. Traumatic dental injuries are most often the result of direct impact and in 90% of cases affect the incisors and/or canines. This is a particular problem when it comes to the permanent dentition in children. Child trauma is not a rare phenomenon, which also determines the existence of the International Association of Dental Traumatology (IADT). The clinical protocol and the quick reaction of the parents are some of the reasons for the successful treatment and follow-up of a case two years after injury. On our recommendation, the tooth is placed in fresh milk until the child arrives at the clinic. The time from avulsion to splinting is 5 hours as the patient is traveling from a remote location. The special thing in this case is that the child suffers from epilepsy, which was not reported by the parents during the interview and taking the anamnesis data. Aim: The aim of the study is to present a clinical protocol and multidisciplinary management of a case with avulsed 11 and its reimplantation of child with epilepsy. Methods: The socio-medical aspect of treatment includes rehabilitation and prevention after a functional and aesthetic solution to the problem. Endodontic and orthodontic treatment was performed. Results: The success for the reimplantation of avulsed 11 can vary depending on several different factors, including the patient’s overall health, hygiene, habits and cooperation. The child is currently being treated with a Shwartz appliance and is being monitored for ankylosis and inflammatory changes. Conclusion: In order to make a comprehensive assessment of the case, it is worth mentioning that this is the child's first encounter with a dentist in life. The reimplantation is a predictable technique and long-term prognosis is not a problem, associated with a high survival rate worldwide.
Avulsed tooth, Reimplantation, Endodontic treatment, Epilepsy, Orthodontics.
The case describes a successful reimplantation and restoration with the same tooth in an avulsed anterior tooth region of a 9-year-old boy with epilepsy. This is the beginning of the third year of follow-up.
Dento-alveolar trauma is considered high risk for the age group of 6 to 18 years. Traditionally, avulsion and reimplantation have poor long-term survival as a result of root resorption and ankylosis. Avulsion, fractures of anterior teeth are reported in 0-3% of all dental injuries [1,2,3,4]. In an avulsion, the tooth may be displaced extraorally, become lodged in the soft tissues of the mouth, esophagus, or nose, or be aspirated. This condition is life-threatening for the child. When an avulsed tooth cannot be located, the patient should be seen in an emergency department to avoid potential respiratory complications. After avulsion and reimplantation, teeth are at risk of infection and root resorption. It can affect negatively reimplantation success and survival. Prevention of the natural dentition, functionally and esthetically, is of particular priority. Treatment alternatives such as fixed prosthetic structures or implants are unacceptable in relation to the child's growth. This case describes the work of an extremely simplified reimplantation in which just two doctors are responsible for the successful treatment. The clinical protocol includes a multidisciplinary approach – surgical, orthodontic and endodontic treatment. The clinical protocol begins with clear instructions for storing the extracted tooth until the patient arrives at the clinic. They refer to the fact that the tooth should not remain dry. The total length of dry storage time has an extremely adverse effect on the success of dental reimplantation. The tooth should only be held by the crown when touched, not soiled, grasped with gauze, rubbed or cleaned. The goal is to preserve the periodontal ligament to revascularize the reimplanted tooth. At the same time, the cooperation of the child and the parents is very important, because results are not compromised by biting food or additional injuries by mistake. The cause of the avulsion is a fall from a bicycle, after which the child hits his mouth on the pavement. One tooth was expelled without traumatic damage to the others. The underlying soft tissues have laceration-contusion wounds. The special thing in this case is that, despite taking anamnestic data, the parents did not report that the child suffered from epilepsy. This was subsequently recorded.
In the literature, there are data on various methods and clinical protocols for traumatic dental injuries in childhood. This presents a challenge due to the diversity of results that these reports summarize. The essence of the review in the literature is expressed not only in the search for the points of contact in patients with dental reimplantation, but also in presenting a scenario in case of rejection and various barriers related to successful treatment. Results from several systematic reviews have shown survival rates to be 75%-98% [5-10].
The presence of temporary teeth The clinical decision depends on the root structure, crown strength, risk of ankylosis, mobility. In many cases, temporary teeth are deliberately left in the mouth to preserve the alveolar bone, even though they can be quite destroyed. But, since the size of the root in them is smaller than that of the permanent tooth, and often compromised, in connection with resorption during growth, it is imperative to make a comprehensive assessment of whether the tooth will remain in the mouth.
Replacement of missing teeth is done with dental implants. They are a suitable solution option in adult patients, but not in children, as the individual is expected to reach skeletal maturity from 18 to 25 years, depending on the type of growth. Most related to children, surgical treatment consists of applying a local anesthetic and reimplantation.
A similar conclusion is made when choosing removable and fixed prosthetic appliances in childhood i.e, they are inapplicable. If a removable prosthetic structure is used, it must be replaced several times, since its use depends on the speed of physical growth in the child. There is a risk of it being broken, lost or swallowed. Fixed dentures to replace lost teeth are more common. For example, a Maryland bridge or a cantilever. Risks are associated with detachment or wear that requires refabrication. So, the patient should pay twice for laboratory and it can affect physician-patient relationship [13,14].
Various orthodontic appliances may be used to restore dentition after trauma. They are generally divided into removable and fixed. Age and aesthetics are decisive until full recovery. It is not intended to close a space, on the contrary, it provides one for the restoration of the bone and, accordingly, for the aesthetics. Bone loss due to space closure with fixed appliances most often results in loss of esthetics. Orthodontic treatment in this case is expressed in a fixed retainer in the first three months, responsible for the immobilization of tooth 11 and subsequent treatment with a Shwartz appliance due to other specific indications. Orthodontic treatment is actually a prelude to the final solution of the clinical problem with an implant. It is a prevention in the prediction of loss of aesthetics during growth [15-18].
When reviewing the scientific literature, it was found that different authors present a variety of data regarding the success and durability of dental restoration treatment. One of the essential problems actually appears precisely in the diversity of the different clinical protocols. What are the most important results? Not coincidentally, Kenny published An International Approach to Core Outcomes Development in Dental Traumatology. What makes a high survival rate of 75% to 100% in long-term follow-up of clinical cases is that the transplant has maintained its vitality throughout the years, that endodontic treatment has been successful, that there is no evidence of complications related to root resorption, ankylosis, etc. Survival is defined as the proportion of teeth that are present in the mouth at a given time after transplantation.The search was conducted using the following search terms in the database of Web of Science (WoS-CC): “Avulsion, Tooth OR “Avulsions, “Avulsed Permanent Teeth” OR “Avulsed Permanent Tooth” OR “Dental Avulsion” OR “Teeth Avulsion” OR “Avulsed Teeth” OR “Knocked Out Teeth” OR “Knocked Out Tooth”, “Replantations, Tooth” OR “Tooth Replantation” OR “Teeth Replantation" OR “Tooth Replantations” OR “Teeth Replantations” OR “Reimplantation, Tooth” OR “Reimplantations, Tooth” OR “Tooth Reimplantation” OR “Tooth Reimplantations” OR “Tooth Reimplant” OR “Teeth Reimplant.” Articles focusing on aspects of the avulsion of permanent teeth were included [8,10,19,20]. Data on reimplantation survival are presented in Table 1.
The patient is a 9 year old boy. The treatment and follow-up of the case took place in a dental clinic in the city of Plovdiv. On arrival in the late evening (11pm) the avulsion of tooth 11, lacerated wounds and labial drainage without fractures of the adjacent teeth were noted. In this case of avulsion, the tooth is completely outside the alveolus. The patient showed an Engle class 1 malocclusion and midline deviation. The clinical protocol and treatment methods were tailored to the child's age and general condition. Reimplantation was possible because the tooth was whole and well preserved in milk according to the instructions. It is assumed that its root surface has not been touched in order to prolong the health of the periodontal ligament. The tooth had complete root development. Alternative treatment with prosthetic structures and implants was rejected given the patient's age. The patient photographs are presented at Figure 1.
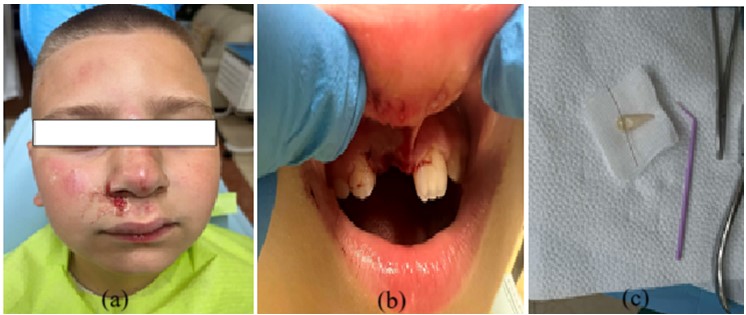 Figure 1: A,B): Extra and intraoral photographs of the patient before the surgery; c): The tooth and some tools used in the procedure.
Figure 1: A,B): Extra and intraoral photographs of the patient before the surgery; c): The tooth and some tools used in the procedure.
The patient's parents reported after several visits, rather than at the initial time of history taking, the comorbidity of epilepsy. Local anesthesia was administered and the tooth was implanted into the alveolus. The tooth was fixed with a doubletwisted orthodontic wire that was adjusted in the patient's mouth. Orthodontic adhesive and photopolymer, well known in practice, were used to meet the requirements for durability. In fact, the technique is similar to that used when adjusting and bonding a fixed orthodontic retainer for the lower jaw. After achieving the optimal relationship of the teeth in the bite and removing the excess material and smoothing the surfaces, the teeth were ligated with a figure-of-eight ligature (φ - 0.4). In Figure 1, it can be seen that the cutting edges of the reimplanted tooth 11 did not match that of 21, which was of concern in terms of revascularization and esthetics. The need for an additional soft wire ligature was assessed. The ligature was additionally glued at several points vestibularly and orally, as we judged that the crowns of the teeth lacked a pronounced equator and could be swallowed. The patient was discharged for home treatment after the appointment of an antibiotic. Given the remote location where the patient lives and for the parents' peace of mind, telephone contact was maintained in the following days. In summary, it was reported that the child was doing well and had no complaints.
In the following three months, the patient visited the office several times. When taking the oral status, no visible changes were noticed on the mucous membrane, there is no swelling, pain or other symptoms suggesting an inflammatory process. The fixed and figure-of-eight ligatures were removed and impressions were taken to make a removable orthodontic appliance. Meanwhile, only tooth 11 had an intrusion ligature adjusted, which significantly leveled the cutting edges of the two central incisors. The intrusion ligature is the author's own and will be presented in a further discussion. Some photos that show the essence of the process are presented at Figure 2.
Figure 3 shows the patient extraorally after two years of observation. During this time, endodontic treatment and an adjusted removable appliance were performed to provide additional bone growth and avoid tooth crowding. It’s visible that the patient is happy, the trust for life is gained, which was actually one of our long-term goals. As the discussion below, it’s the first encounter with a dentist in life.
In these three years the patient follows the doctor requirements not to include the tooth 11 in the biting process and to avoid foods and drinks with high range of temperature.
There is no consensus in the literature on the method of fixation. Fixation with a rigid wire is considered the most effective method. In the long term period, this can lead to ankylosis. In the current case, fixation was performed with a hard wire for three months, after which it was removed and work continued with the placement of Schwartz appliance due to other specific indications, which will promote bone regeneration and healing of the bone and periodontal ligament.
In conclusion, it can be argued that the reimplantation technique is a predictable technique and long-term prognosis is not a problem related to the high survival rate worldwide. Not without importance is the assessment of teeth that have not completed development. A clear surgical protocol should be followed and the patient should be followed up at six months. In order to be able to evaluate the effectiveness of the applied treatment, follow-up time is needed. We are happy to have helped.
We would like to thank all parents who participated in this sociological study.
None declared.
