 Journal of Medical Research and Surgery
PROVIDES A UNIQUE PLATFORM TO PUBLISH ORIGINAL RESEARCH AND REMODEL THE KNOWLEDGE IN THE AREA OF MEDICAL AND SURGERY
Journal of Medical Research and Surgery
PROVIDES A UNIQUE PLATFORM TO PUBLISH ORIGINAL RESEARCH AND REMODEL THE KNOWLEDGE IN THE AREA OF MEDICAL AND SURGERY
 Journal of Medical Research and Surgery
PROVIDES A UNIQUE PLATFORM TO PUBLISH ORIGINAL RESEARCH AND REMODEL THE KNOWLEDGE IN THE AREA OF MEDICAL AND SURGERY
Journal of Medical Research and Surgery
PROVIDES A UNIQUE PLATFORM TO PUBLISH ORIGINAL RESEARCH AND REMODEL THE KNOWLEDGE IN THE AREA OF MEDICAL AND SURGERY
 Indexed Articles
Indexed ArticlesSelect your language of interest to view the total content in your interested language
Yogesh Sharad Salphale1* , Aman Tomar2
, Aman Tomar2 , Vikrant G. Salphale3
, Vikrant G. Salphale3 , Atharva Sharma4
, Atharva Sharma4 , Gopal Shinde5
, Gopal Shinde5
1Consultant Orthopaedic Surgeon, Shushrusha Multispecialty Hospital, Lane Opp. Z.P, Chandrapur, Maharashtra, India.
21st Year Resident, Department of Orthopaedic, SBKS Medical Institute and Research Centre, Vadodara, Gujarat.
3Senior Physiotherapist, Shushrusha Multispecialty Hospital, Lane Opp. Z.P, Chandrapur, Maharashtra, India.
4Junior Resident, HBT Medical College And Dr. R N Cooper Hospital, Juhu, Mumbai, Maharashtra, India.
5Associate Professor, Department of Orthopaedics, Maharashtra Post Graduate Institute of Medical Education and Research , Maharashtra University of Health Sciences, Nashik, Maharashtra, India
Correspondence to: Yogesh Sharad Salphale, Consultant Orthopaedic Surgeon, Shushrusha Multispecialty Hospital, Lane Opp. Z.P, Chandrapur, Maharashtra, India.
Received date: October 26, 2023; Accepted date: November 13, 2023; Published date: November 20, 2023
Citation: Salphale YS, Tomar A, Salphale VG, et al. An Unusual Combination of Subtrochanteric Fracture Associated with Ipsilateral Posterior Dislocation of Hip: A Case Report. J Med Res Surg. 2023;4(5):108-111. doi: 10.52916/jmrs234120
Copyright: ©2023 Salphale YS, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted
use, distribution and reproduction in any medium, provided the original author and source are credited.
Background: A unique fracture pattern involving subtrochanteric fracture associated with ipsilateral posterior dislocation of hip in a young adult male eventually having a functional hip at six year follow up following aggressive management is described. Case presentation: We present a case of a 40 year old male labourer from Central India who was admitted in our hospital within hours of a road accident he sustained in Feb 2012. Early reduction and osteosynthesis, supervised physiotherapy, and routine follow-up all contributed to the patient having an acceptable functioning hip at the six-year follow-up. Conclusion: The result at six year follow up showed complete union of fracture without any radiological signs of avascular necrosis of the femoral head which highlights the importance of team work in the management of the complex injury.
Subtrochanteric fracture, Ipsilateral posterior dislocation of hip, Proximal femoral nailing, Physiotheraphy, Hip dislocation.
A unique fracture pattern involving subtrochanteric fracture associated with ipsilateral posterior dislocation of hip in a young adult male eventually having a functional hip at six year follow up following aggressive management is described. In car crashes, the flexed lower extremity impacts against the dashboard, leading to knee, thigh, and hip injuries. The consequence of an anteroposterior force applied to the lower extremity differs depending on the location of the contact and the position of the leg at the time of impact, which dislocates the femoral head.
When anteroposterior force is applied to a flexed and internally rotated femur, the femur dislocates superiorly and posteriorly from the acetabular cup causing a hip dislocation.
When the hip is abducted only slightly, the posterior dislocation of the hip joint may be accompanied by a fracture to the acetabular wall or the femoral head [1].
It is common knowledge that posterior hip dislocation can occur in conjunction with a fracture of the head of the femur, the acetabulum, or the trochanter [1-3].
The combination of a subtrochanteric fracture and an ipsilateral posterior hip dislocation is an uncommon occurrence that, to this day, has not been recorded in the medical literature.
The goal of this study is to describe our experience with successfully treating a rare injury by performing a closed reduction of the dislocation and osteosynthesis of the subtrochanteric fracture. Additionally, we will briefly go through the relevant literature and treatment choices.
A male labourer from Central India who was 40 years old and had been involved in a traffic accident in February 2012 was brought to our hospital within hours of the incident, On examination he was conscious but was unable to move his left lower limb which was 4 cm shorter than the right and was rotated externally. A localised swelling was observed in the area surrounding the left gluteal region. There were no obvious signs of injuries on the outside. There were no injuries to the internal organs. Radiographs showed that the patient had a subtrochanteric fracture in conjunction with an ipsilateral posterior dislocation of the hip (Figure 1a). Figure 1b shows the results of a three-dimensional CT reconstruction of the pelvis. The flexed and internally rotated position of the proximal dislocation fragment, which included the head, neck, and a portion of the trochanter, was noted. There was no sign of a fracture in either the head or neck component, as well as the acetabulum. The sciatic nerve was unharmed, and he showed no signs of vascular damage.
 Figure 1a: A radiograph showing subtrochanteric fracture associated with ipsilateral posterior dislocation of hip.
Figure 1a: A radiograph showing subtrochanteric fracture associated with ipsilateral posterior dislocation of hip.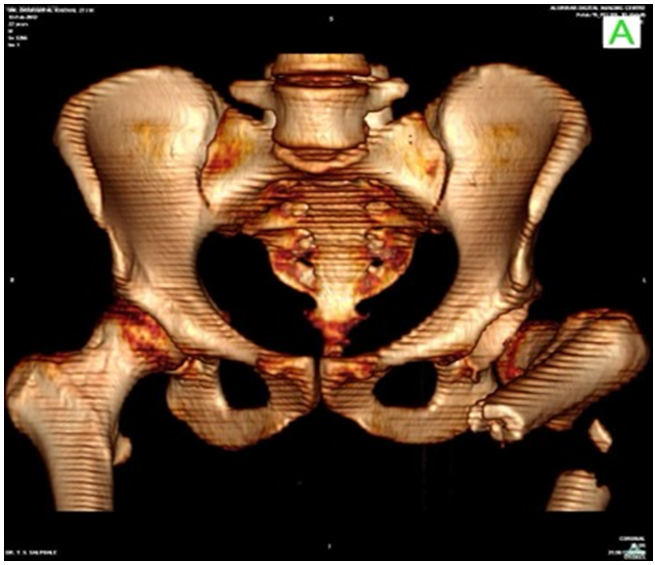 Figure 1b: A 3D CT reconstruction showing the injury pattern with communition and associated with post dislocation of the hip.
Figure 1b: A 3D CT reconstruction showing the injury pattern with communition and associated with post dislocation of the hip.As the patient was moved to the emergency operating theatre, under spinal anaesthesia, a trial of closed reduction employing a schanz pin as a joy stick into the trochanter was tried. After that, the hip was repositioned by applying a moderate pressure to the Schanz pin, and manually lifting the proximal fragment in a gentle manner. All of this was done in order to relocate the hip. The nature of the reduction was evaluated under the C arm, where it was found to be concentric.
The subtrochanteric fracture was reduced using closed manipulation, and a proximal femoral nailing was performed using one dynamically locked screw while the patient was under the same anaesthesia. Following surgery, the patient was started on an individualized physiotherapy programme that was carried out under the direction of the staff physiotherapist. A regimen of static quadriceps and abductor strengthening was initiated as soon as the post operative pain subsided. Subsequntly he was instructed to walk non weight bearing ,continuing with the exercises with increasing loads to strengthen the quadriceps.He complied with the instructions and was discharged.
He presented to our unit after 8 months when he had a fall. The non union with broken implant was seen on the radiograph (Figure 1c).
He underwent a second operation in which a PFN and two distal screws were inserted.At the site of the nonunion, bone grafting was performed. After the fracture had healed, he began having follow-up appointments once per year. Previously, these appointments occurred every two months. After a period of six years, the patient's hip was completely pain-free, and the fracture had successfully healed. He was able to carry out the things that were necessary for his daily living. There were no indications of avascular necrosis found on the radiographs (Figure 1d).
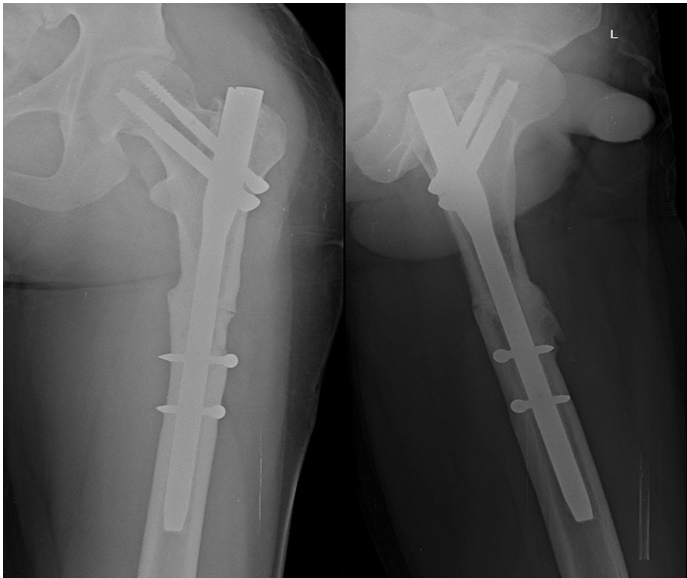 Figure 1d: Showing follow up x-ray at 6 years follow up with well consolidated fracture (arrow) with no evidence of osteonecrosis of the femoral head.
Figure 1d: Showing follow up x-ray at 6 years follow up with well consolidated fracture (arrow) with no evidence of osteonecrosis of the femoral head.Accidents involving motor vehicles are leading to an increase in the incidence of critical orthopaedic conditions, such as acute hip dislocation and fracture-dislocation of the hip. At the moment of impact, the position of the hip, the vectors, and the amount of force all contribute to determining the direction in which the hip will dislocate [1]. The early identification and reduction of the dislocation are the two most important factors in effective management. A delay in detecting and taking preventative measures against the risk of complications and morbidity can lead to negative outcomes. The severity of the damage, the amount of time that passed between the injury and the reduction, the type of fracture or dislocation, the acetabulum–femoral head articulation congruency, and the adequateness and longevity of the reduced hip joint are all prognostic indications [3].
Because of the secondary pull of the iliopsoas, gluteus medius, and short external rotators on the proximal fragment, subtrochanteric fractures have an intrinsic instability. This causes substantial fracture displacement, dragging the segment into flexion, abduction, and external rotation. In addition, the unopposed pull of the adductors on the distal part of the femur frequently results in the femoral shortening and adduction. It is necessary to overcome these deforming stresses in order to achieve anatomical reduction thereby preventing major problems and poor clinical outcomes such as failed fixation, shortening, malrotation, and non-union.
In order to regain maximal ambulatory capability, it is necessary to restore femoral length and rotation in addition to femoral head and neck angulation in order to achieve enough abductor tension and strength.
Hip reduction and temporary femur fixation with the use of an external fixator have both been tried as potential treatments for traumatic posterior hip dislocations that are accompanied with ipsilateral femur shaft fractures. Later on the shaft fracture is repaired using an interlocking nailing [4]. It has been reported that a combined subtrochanteric femur fracture along with an anterior hip dislocation can be treated by performing a closed reduction of the dislocation and making use of an external fixator until the patient is stabilised and then doing interlocking nailing. Our case, which had a subtrochanteric fracture with posterior dislocation was taken to the emergency OR and the procedure of closed reduction of the posterior dislocation and proximal femoral nailing for the subtrochanteric fracture, in the same OR setup was carried out without much difficulty after the patient was stabilised.
The femur is thrust upwards during the dashboard injury, causing the femoral head to dislocate. This results in the femoral head carrying a piece of bone, which is typically from the posterior wall of the acetabulum, which causes a fracture dislocation. When a seatbelt is used and the hip is in an adducted position at the time of damage, a pure dislocation occurs. However, when the hip is in a neutral position or an abducted position at the time of injury, a dislocation occurs together with a fracture of the femoral head or acetabulum.
Since the neck was unharmed, the previously described method does not apply to the circumstances of this incident. We believe that our patient's posterior hip dislocation and subtrochanteric fracture were caused by a longitudinal compression force, adduction, and posterolateral force acting across the trochanteric region.
The classification systems that have been described for hip dislocation injuries [4,5] have not been able to provide an explanation for this pattern of fractures.
This case presentation is important because such an injury is rare but are anticipated to become more widespread, which will necessitate revising the current classifications for the mechanisms that cause hip dislocation. We hypothesize that longitudinal force with adduction precedes internal rotation or upper thigh damage.
In order to avoid the morbidity that is typically associated with complex injuries, it may be necessary to perform open reduction and internal fixation as soon as possible after the damage has occurred.
This highlights the aggressive approach of the reduction and fixation of the antecedent fracture once the patient is stabilised, as well as the importance of avoiding distraction at the fracture site, which could jeopardise the eventual result.
The authors have no conflicts of interest to report.
No
