 Journal of Medical Research and Surgery
PROVIDES A UNIQUE PLATFORM TO PUBLISH ORIGINAL RESEARCH AND REMODEL THE KNOWLEDGE IN THE AREA OF MEDICAL AND SURGERY
Journal of Medical Research and Surgery
PROVIDES A UNIQUE PLATFORM TO PUBLISH ORIGINAL RESEARCH AND REMODEL THE KNOWLEDGE IN THE AREA OF MEDICAL AND SURGERY
 Journal of Medical Research and Surgery
PROVIDES A UNIQUE PLATFORM TO PUBLISH ORIGINAL RESEARCH AND REMODEL THE KNOWLEDGE IN THE AREA OF MEDICAL AND SURGERY
Journal of Medical Research and Surgery
PROVIDES A UNIQUE PLATFORM TO PUBLISH ORIGINAL RESEARCH AND REMODEL THE KNOWLEDGE IN THE AREA OF MEDICAL AND SURGERY
 Indexed Articles
Indexed ArticlesSelect your language of interest to view the total content in your interested language
Saikou Yaya Diakité1* , Fodé Lansana Camara 2, Sandaly Diakité3, Habiboulaye Baldé2, Ibrahima koussy Bah4, Alpha Madiou Barry2, Thierno Illah Barry2, Zakaria Sow2, Hamidou Sylla2, Biro Diallo2
, Fodé Lansana Camara 2, Sandaly Diakité3, Habiboulaye Baldé2, Ibrahima koussy Bah4, Alpha Madiou Barry2, Thierno Illah Barry2, Zakaria Sow2, Hamidou Sylla2, Biro Diallo2
1Department of Visceral Surgery, Conakry Regional Hospital/Faculty of Health Sciences and Techniques-Gamal Abdel Nasser University of Conakry,
Guinea
2Department of Visceral Surgery, Donka National Hospital/Faculty of Health Sciences and Techniques-Gamal Abdel Nasser University of Conakry,
Guinea
3Department of General Surgery, Ignace Deen National Hospital/Faculty of Health Sciences and Techniques-Gamal Abdel Nasser University of
Conakry, Guinea
4Department of Gynecology-Obstetrics, Ignace Deen National Hospital/Faculty of Health Sciences and Techniques-Gamal Abdel Nasser University
of Conakry, Guinea
Correspondence to: Saikou Yaya Diakité, Department of Visceral Surgery, Conakry Regional Hospital/Faculty of Health Sciences and Techniques-Gamal Abdel Nasser University of Conakry, Guinea
Received date: February 13, 2023; Accepted date: March 16, 2023; Published date: March 23, 2023
Citation: Diakité SY, Camara FL, Diakité S, et al. Acute Generalized Post-Cesarean Peritonitis Complicated by Abdominal Gangrene at Conakry University Hospital: A Case Report. J Med Res Surg. 2023;4(2):22-26. doi: 10.52916/jmrs234101
Copyright: ©2023 Diakité SY, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted
use, distribution and reproduction in any medium, provided the original author and source are credited.
Purpose: To discuss the difficult diagnosis of a rare case of post-cesarean peritonitis complicated by abdominal wall gangrene. Case Report: Mrs. A.D, 25 years old, admitted on 9/24/2018 for fluid flow through the operative wound, abdominal pain, fever, cough. Evolution 6 days. Onset: edema, redness, blisters of the abdominal wall then fluid flow through the surgical wound of a cesarean section (breech presentation) at 38 weeks, performed on 9/15/2018 in a medico-communal center in Conakry. Patient readmitted on D6: abdominal necrosis+blisters: dressing of the operative wound, Ampicillin 1 g, Perfalgan 1 g then referred to visceral surgery at Donka National Hospital. No specific background. No known allergy. Use of dermocorticoids for skin depigmentation. G2, P2, Cesarean section 1, Alive 1, Died 1. Patient conscious, hypocoloured in teguments and conjunctivae: BP=110/70 mm Hg, pulse=104/min, FR=24 cycles/min, temperature=37.8°C. Abdomen: wound extending from the hypogastrium up to 3 cm above the umbilical bone, also involving the flanks, with necrotic background+foul-smelling whitish pus. TV: vulva covered with sero-hematic secretions. Leukocytes 16 G/l Hb 9 g/l VS accelerated. At laparotomy: necrotic areas of the skin at the parietal peritoneum, discharge of 1 liter of foul-smelling purulent fluid. Then midline above and below umbilical incision connecting the transverse incision: deposits of fibrin throughout the cavity, intact uterine sutures: removal of fibrin. Peritoneal toilet. Aponeurotic approximation. Stripping of necrotic tissue. Parietal washing, dressing. Peritoneal fluid: Staphylococcus aureus, ceftriaxone 1 g IV twice a day. postoperative follow-up: iterative necrosectomies, complete healing on postoperative eventration. Conclusion: Possibility of post-cesarean peritonitis with progression to abdominal gangrene.
Peritonitis, Cesarean section, Abdominal gangrene
Acute generalized post cesarean section peritonitis is a surgical emergency with a serious prognosis [1]. Its evolution towards parietal gangrene can be fulminant and thus constitute one of the major parietal complications, exceptional of caesarean section [2]. The use of dermocorticoids is a pejorative risk factor in the occurrence of gangrene [3]. The aim of this case report was to discuss a difficult diagnosis of a rare case of post-caesarean peritonitis complicated by gangrene of the abdominal wall on a site of voluntary skin depigmentation.
Mrs. A.D, 25 years old, shopkeeper, admitted on 24/9/2018 for fluid discharge through the operative wound, abdominal pain, fever, cough. Evolution 6 days. The history highlights a progressive onset marked by the occurrence of edema, redness, phlyctenes of the abdominal wall and then a liquid discharge through an operative wound of a caesarean section for breech presentation at 38 SA, performed on 15/9/2018 in a medicalcommunal center of Conakry, accompanied by abdominal pain of burning type, fever, productive cough and dyspnea. This picture settled at D4 postoperative after discharge from the clinic. She was readmitted at D6 with abdominal necrosis and phlyctenes. She benefited from local care (dressing of the surgical wound), ampicillin 1 g times 3/D, Perfalgan 1 g every 4 hours) without improvement. On the same day, she was referred to the visceral surgery Department of the Donka National Hospital of Conakry for treatment.
No particular history. No known allergy. Use of dermocorticoids for voluntary skin depigmentation for the duration of 2 years. Gestité 2, Parité 2, Césarienne 1, Vivant 1, Décédé 1(mort-né) On examination: conscious patient, poor general condition: hypo colored integuments and conjunctiva, writhes with abdominal pain; BP=110/70 mm Hg, pulse=104/mn, FR=24 cycles/mn, temperature=37.8°C; Abdomen participates in breathing, seat of a wound going from the hypogastrium to 3 cm above the umbilical, also involving the flanks, with a necrotic bottom letting out whitish nauseating pus, preserved prehepatic dullness, no sloping dullness of the flanks, audible peristalsis (Figure 1).
TV: dirty vulva covered with serohematic secretions, short median neck open to the finger pad surmounted by an enlarged uterus, the lateral cul-de-sacs were free. The finger pad returned with traces of blackish blood. TR: anal margin free, anal sphincter normo tonic, rectal ampulla contains soft stool, douglas painful and bulging; finger pad returns with traces of normal looking stool. Elsewhere no particularities. Clinical diagnosis: abdominal gangrene on a ground of skin depigmentation.
Biology: hyperleukocytosis 16 G/L with neutrophils Hb level: 9 g/L VS accelerated, blood glucose: 1 g/L urine dipstick without any particularities. We were unable to perform an imaging examination because of the noisy abdominal gangrene and its non-availability in emergency at the Donka National Hospital.
Under general anesthesia with orotracheal intubation. Transversal incision under the umbilical skin and subcutaneous cellular tissue, necrotic areas extending from the skin to the parietal peritoneum were noted. When the abdominal cavity is opened through the operating wound (Pfannenstiel), a liter of foul-smelling, cloudy fluid flows out. This leads to a median incision above and below the umbilicus, connecting the transverse incision (Figure 2). Exploration reveals fibrin deposits throughout the cavity. Dilatation of the small intestines. The uterine sutures were intact. Actions: removal of fibrin. Peritoneal cleansing with 3 liters of 0.9% SS. Fastening of the aponeurosis. Stripping of necrotic tissues involving the large muscles, the rectus abdominis, the subcutaneous cellular tissue, and the skin. Parietal lavage with 1.5 liters of 0.9%; wicks soaked in hydrogen peroxide.
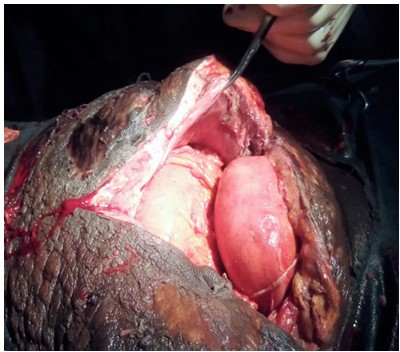 Figure 2: Operative view Necrosis of the infiltrated abdominal wall, erosive inflammatory skin placards, dilated bowels.
Figure 2: Operative view Necrosis of the infiltrated abdominal wall, erosive inflammatory skin placards, dilated bowels.Bacteriological analysis of the peritoneal fluid revealed Staphylococcus aureus. A treatment made of ceftriaxone IV 1 time/d during 5 days. Relay: amoxicillin+clavulanic acid 1 g associated with metronidazole 500 mg Perfalgan 1 g times 3/d, tramadol 100 mg times 2/d rehydration 1.5L/24 h (Ringer Lactate 500 mg, SS9% 500 mg, SG5% 500 mg).
The postoperative follow-up was clinical and biological. Repeated clinical examinations of the patient noted areas of necrosis of the abdominal wall which were treated by iterative necrosectomies under sedation during daily dressings (Figure 3 and 4).
The biological control noted an improvement of the biological inflammatory syndrome. At D15 postoperatively, the patient developed a sub-occlusive syndrome (abdominal pain, vomiting, cessation of feces and incomplete gas) which was treated with Prostigmine. At D90 (3 months) we noted a good clinical and biological evolution: good evolution of the wound (Figure 5) and complete healing of the wound on postoperative ventration (Figure 6).
Caesarean section is one of the common surgical procedures in obstetrics [4]. After cesarean section, the main etiologies of infectious complications are parietal endometriosis, urinary tract infections, infections of the operative scar and of the peritoneal cavity [1]. Post Caesarean Section Peritonitis (PCP) can develop into gangrene of the abdominal wall [1,4]. In this case, PCP is an integral part of deep surgical site and peritoneal cavity infections according to the Centers for Diseases Control (CDC) and prevention classification [5,6]. According to a systematic review, 13.5 to 94.8% of surgical site infections occur after cesarean section [4,5]. The average time to detection of abdominal infection after cesarean section is variable. In the literature, this delay does not exceed 15 days [4,6]. In our case, peritonitis complicated by gangrene was detected after 6 days post caesarean section. Merzougui, et al. [1] in Tunis reported a delay of 9.5 days.
The risk factors for the occurrence of post caesarean abdominal infection are related to the degree of bacterial contamination, the general conditions of the patient and the factors related to the surgical procedure [1,5]. In our case, the main risk factor related to the patient was the use of dermocorticoids for voluntary skin depigmentation. Indeed, dermocorticoids can be responsible for side effects dominated by skin atrophy, skin tears caused by the slightest trauma, large superficial erosions and delayed healing, subcutaneous hemorrhages and even superficial necroses [3]. The risk factors related to the operation in the literature are the degree of urgency (urgent, scheduled), the duration of the operation, the type of anaesthesia (Rachi anaesthesia, general anaesthesia), the type of incision (median, Pfannestiel), the degree of contamination, antibiotic prophylaxis [1,7]. In our observation these factors could be the presentation of the site which can increase the risk of venous thromboembolic accidents [8], the clean -contaminated character of the operation (stage II of Alteimeier's classification) [6].
The diagnosis of gangrene was clinical (Figure 1) as described in the literature [2,4]. In the early stage (stage I), the symptoms are edema, erythema, and warmth, with the main sign being pain on palpation [4]. The lack of specificity at this stage makes the diagnosis difficult, with its corollary of delayed management [4]. It is in stages II and III that the local signs become clearer with painful infiltrated areas, necrosis, and subcutaneous crepitations. The general signs are indicative of sepsis (hypotension, tachycardia, polypnea) [4]. In our case, the patient was admitted in stage III of gangrene with extensive necrosis of the anterolateral wall of the abdomen and a purulent discharge through the Pfannenstiel incision (Figure 1). We did not perform imaging examinations because they were not available in the emergency room at Donka Hospital.
The biological work-up showed an inflammatory biological syndrome which confirmed the cutaneous infectious process consecutive to the intra-abdominal sepsis, anemia which are paraclinical signs of severity of the abdominal infection [5,6]. In front of the noisy picture of gangrene, it was clinically difficult to evoke the diagnosis of acute generalized peritonitis. Ultrasound or CT scan of the abdomen would certainly have revealed a liquid intraperitoneal effusion and described the lesions of the abdominal wall planes [7].
The diagnosis of peritonitis was made intraoperatively upon observation of purulent fluid, deposition of false membranes throughout the peritoneal cavity. The uterine sutures were intact with no other macroscopic visceral lesions. The same observation was made by Merzougui, et al. [1] who noted 1 case of post caesarean peritonitis in a 32 year old patient, Gestité 2 Parity1 Abortion 0 who had a caesarean section for acute fetal distress at 42 weeks of amenorrhea. The evolution was favorable [1]. In our case, the etiological hypotheses of this abdominal infection could be cutaneous (bacterial inoculation during the incision on a skin weakened by skin depigmentation), genital (vulvovaginitis), peritoneal (fulminant infection of the peritoneum). Indeed, the opening of the uterine cavity for the extraction of the fetus, the flow of amniotic fluid would be factors of contamination of the abdominal wall already weakened by the erosive effects of the depigmentation. This contamination would have eventually reached the peritoneal cavity, responsible for the peritonitis complicated by gangrene of the abdominal wall. Another hypothesis could be insufficient intraoperative asepsis in the operating room, as suggested by other authors [1,6]. The germs responsible for these abdominal infections come from the flora of the skin or the mucous membranes affected (uterine mucosa) during the caesarean section [9]. In our case, analysis of the purulent peritoneal fluid allowed the isolation of staphylococcus aureus. The latter is the first germ in all surgical sites except for abdominal surgery where gram-negative bacteria predominate [9].
The treatment of post caesarean peritonitis complicated by gangrene is surgical [10]. The therapeutic attitudes are diverse and depend on the clinical context. Lazar, et al. [10] reported a case of reconstruction by skin grafting for large losses of skin substance. Martin, et al. [11] used an abdominal advancement flap for the treatment of extensive necrosis of complex topography. In our case, the treatment consisted of necrosectomies in addition to adhesiolysis and peritoneal lavage. Post-operatively, the necrosectomies were iterative and responsible for large losses of abdominal wall substances. In addition to surgery, the antibiotic treatment recommended by the French National Authority for Health (HAS) in cases of severe necrosis caused by staphylococcus aureus is a combination of cefazolin (100 mg/kg/d in three doses) and clindamycin (40 mg/Kg/d in three doses). In our case we used a combination of ceftriaxone 1 g every 12 hours and Metronidazole 500 mg every 8 hours. Antibiotic prophylaxis is useful in reducing the incidence of parietal and intraperitoneal infectious complications [1,4,6]. Post-operative therapeutic follow-up allowed a slow but complete healing to be obtained after 3 months without having to resort to a skin graft as in the observation of Lazar, et al. [10]. This directed healing resulted in the occurrence of a postoperative eventration (Figure 6) which will be treated very soon (we are considering a cure with prosthesis).
This is a surgical emergency that can be life-threatening. Our observation allowed us: to pose the problem of etiological diagnosis (cutaneous, peritoneal) of a post caesarian intraperitoneal sepsis in front of an abdominal gangrene. To show the possibility of the existence of a post caesarean peritonitis and to evoke its possible evolution towards abdominal gangrene. In this case, abdominal CT scan could be of capital importance in the preoperative diagnosis of peritonitis in front of the noisy picture of cutaneous gangrene. It can also show the possibility of slow and complete skin healing after iterative necrosectomies.
We have no known conflict of interest to disclose.
No
