 Journal of Medical Research and Surgery
PROVIDES A UNIQUE PLATFORM TO PUBLISH ORIGINAL RESEARCH AND REMODEL THE KNOWLEDGE IN THE AREA OF MEDICAL AND SURGERY
Journal of Medical Research and Surgery
PROVIDES A UNIQUE PLATFORM TO PUBLISH ORIGINAL RESEARCH AND REMODEL THE KNOWLEDGE IN THE AREA OF MEDICAL AND SURGERY
 Journal of Medical Research and Surgery
PROVIDES A UNIQUE PLATFORM TO PUBLISH ORIGINAL RESEARCH AND REMODEL THE KNOWLEDGE IN THE AREA OF MEDICAL AND SURGERY
Journal of Medical Research and Surgery
PROVIDES A UNIQUE PLATFORM TO PUBLISH ORIGINAL RESEARCH AND REMODEL THE KNOWLEDGE IN THE AREA OF MEDICAL AND SURGERY
 Indexed Articles
Indexed ArticlesSelect your language of interest to view the total content in your interested language
Camara FL1* , Balde H1, Barry AM1, Camara SN2, Diakite SY1, Balde AK1, Soromou G1, Sylla H1, Diallo AA1, Toure I1, Balde TM1, Yattara A3, Soumaoro LT1, Toure A1, Diallo AT4, Diallo B1
1Department of Visceral Surgery, Donka National Hospital, Conakry, Guinea.
2Department of Visceral Surgery, Sino-Guinean Friendship Hospital, Conakry, Guinea.
3Department of General Surgery, Prefectural Hospital of Dubreka, Dubréka, Guinea.
4Department of General Surgery, Ignace Deen Hospital, Conakry, Guinea.
, Balde H1, Barry AM1, Camara SN2, Diakite SY1, Balde AK1, Soromou G1, Sylla H1, Diallo AA1, Toure I1, Balde TM1, Yattara A3, Soumaoro LT1, Toure A1, Diallo AT4, Diallo B1
1Department of Visceral Surgery, Donka National Hospital, Conakry, Guinea.
2Department of Visceral Surgery, Sino-Guinean Friendship Hospital, Conakry, Guinea.
3Department of General Surgery, Prefectural Hospital of Dubreka, Dubréka, Guinea.
4Department of General Surgery, Ignace Deen Hospital, Conakry, Guinea.
Correspondence to: Camara FL, Department of Visceral Surgery, Donka National Hospital, Conakry, Guinea.
Received date: July 03, 2023; Accepted date: July 12, 2023; Published date: July 19, 2023
Citation: Camara FL, Balde H, Barry AM, et al. Achalasia of the Esophagus at Donka National Hospital: A Case Report. J Med Res Surg. 2023;4(4):70-72. doi: 10.52916/jmrs234111
Copyright: ©2023 Camara FL, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted
use, distribution and reproduction in any medium, provided the original author and source are credited.
Background: Esophageal achalasia is an esophageal motility disorder of unknown etiology that results in impaired lower esophageal sphincter relaxation and loss of esophageal peristalsis. The aim of our study was to show our experience in the management of esophageal achalasia in a case treated by laparotomy in our service. Case Report: 21-year-old patient, student, admitted to our department for progressive dysphagia to solids accompanied by regurgitation, epigastric pain, nocturnal cough and weight loss, evolving for 5 years. ATCD of pulmonary tuberculosis. The physical examination noted a deterioration in general condition, stage (I) of the WHO; there was hypo coloration of the integuments and conjunctivae, TA=120/80mmHg, Pulse=70/min. The abdomen was symmetrical with presence of sluggish skin folds, supple and painless without a palpable mass, the digital rectal examination did not present any particularity. The thorax was symmetrical with a FR=20 c/mn. The biology showed a normo chrome and normocytic anemia of 8 g/l Group O+. The esogastroduodenal transit was in favor of an amputation (tight stenosis) extended on the cardia with megaesophagus upstream. We performed a cardiomyotomy according to Heller associated with a hemivalve according to Toupet. We performed a followed by preesophageal and subhepatic drainage. The postoperative course was simple, marked by a resumption of food on D6 postoperatively. The control test carried out with gastrographine 10 days after the surgical intervention noted a regression of the signs with passage of the product of contrast in the small intestine. The patient seen again 6 months after the operation showed no particularities. Conclusion: Achalasia is a chronic esophageal motility disorder characterized by the inability of the lower esophageal sphincter to relax. Heller cardiomyotomy by laparotomy associated with Toupet-type fundoplication retains its place in its management in our exercise context.
Esophageal achalasia, Heller cardiomyotomy, Laparotomy.
WHO: World Health Organisation; LES: Lower Esophageal Sphincter; HRM: High-Resolution Manometry; IRP: Integrated Relaxation Pressure; GERD: Gastroesophageal Reflux Disease
Achalasia is a chronic esophageal motility disorder characterized by a lack of peristalsis and the inability of the lower esophageal sphincter to relax [1]. Despite its rarity, it is the most common primary motor disorder of the esophagus with an incidence of 1/100,000 and a prevalence of 10/100,000. First described by Sir Thomas Willis in 1674, its etiology is not yet clear, but it is ultimately a selective disorder of the myenteric plexus (or Auerbach's) inhibitory neurons of the distal esophagus and the lower esophageal sphincter. The clinical symptomatology is that of dysphagia to solids and liquids associated with regurgitation of undigested bland food or saliva, substernal chest pain, weight loss, and sometimes even heartburn [2].
Treatment of achalasia is palliative only and all therapeutic efforts are aimed at facilitating adequate passage through the cardia and, at the same time, preventing late structural and functional esophageal complications.
The aim of our study was to discuss a rare case of esophageal achalasia treated by laparotomy in our department.
21-year-old patient, student, admitted to our department for progressive dysphagia to solids accompanied by regurgitation, epigastric pain, nocturnal cough and weight loss, evolving for 5 years. ATCD of pulmonary tuberculosis. The physical examination noted a deterioration in general condition, stage (I) of the WHO; there was hypo coloration of the integuments and conjunctivae, TA=120/80 mmHg, Pulse=70/min. The abdomen was symmetrical with presence of sluggish skin folds, supple and painless without a palpable mass, the digital rectal examination did not present any particularity. The thorax was symmetrical with a FR=20 c/mn. The biology showed a normo chrome and normocytic anemia of 8 g/l Group O+. The esogastroduodenal transit was in favor of an amputation (tight stenosis) extended on the cardia with megaesophagus upstream. We performed a cardiomyotomy according to Heller associated with a hemivalve according to Toupet. We performed a followed by preesophageal and subhepatic drainage. The control test carried out with gastrographine 10 days after the surgical intervention noted a regression of the signs with passage of the product of contrast in the small intestine. The patient seen again 6 months after the operation showed no particularities.
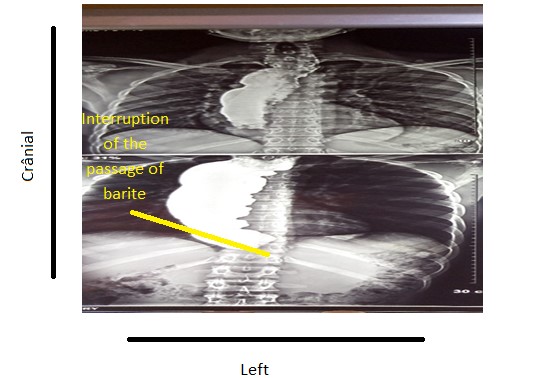 Figure 1: TOGD showing an amputation (tight stricture) extended over the cardia with megaesophagus upstream.
Figure 1: TOGD showing an amputation (tight stricture) extended over the cardia with megaesophagus upstream.
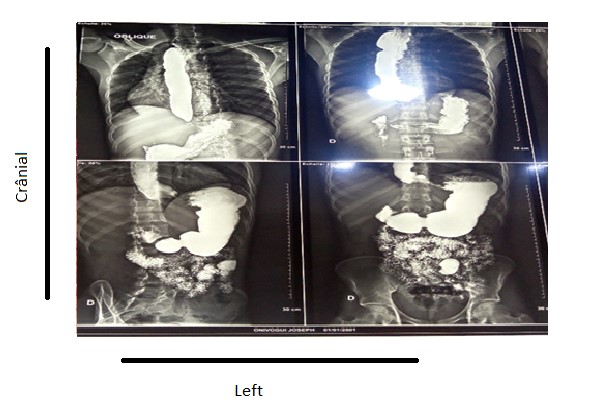 Figure 3: Control TOGD at D10 postoperative showing the regression of signs with passage of the contrast product in the small intestine.
Figure 3: Control TOGD at D10 postoperative showing the regression of signs with passage of the contrast product in the small intestine.
Achalasia occurs due to the absence of peristalsis and is a disorder of the Lower Esophageal Sphincter (LES) that affects both sexes and all ethnicities [3,4]. Our case was a young male subject. The pathophysiology of achalasia is based on the selective loss of inhibitory neurons in the myenteric network, which can interfere with coordination of esophageal peristalsis and relaxation of LES during swallowing [5]. Traditionally, achalasia was diagnosed based on symptoms (dysphagia, regurgitation, chest pain, and weight loss), commonly used tests including barium esophagography, esophageal manometry, and endoscopy. An atonic and dilated esophageal body with a classic "bird's beak" appearance of the gastroesophageal junction on barium swallow and fluoroscopy are typical radiological features. In recent decades, the advent of High-Resolution Manometry (HRM) and standardization based on the Chicago classification has increased the early recognition of the disease [6,7]. Since the launch of the Chicago classification, the diagnosis and management of achalasia have been refined. Additionally, the use of esophageal pressure topography has improved diagnostic accuracy and enhanced early recognition of clinically relevant achalasia subtypes, allowing treatment plans to be tailored according to different subtypes to improve results.
The chicago classification based on High-Resolution Manometric Pressure Topography (HRMPT) distinguishes esophageal motility disorders into 3 subtypes: Type I (classic achalasia) refers to patients with absent peristalsis, no pressurization in the esophageal body and a high Integrated Relaxation Pressure (IRP); Type II (achalasia with compression) refers to patients with absence of peristalsis and contractile activity, pan-esophageal pressurization greater than 30 mmHg and elevated IRP; Type III (spastic achalasia) is associated with absent peristalsis and 2 or more spastic contractions with or without periods of compartmentalized pressurization and high IRP [6].
The TOGD and the eosogastroduodenal fibroscopy were the only diagnostic means of achalasia in our context of exercise. We were unable to classify achalasia according to subtype.
There are several treatment options for achalasia. Medical, endoscopic and surgical. Certain medications have been proven in the non-operative management of Achalasia by reducing the pressure of the lower esophageal sphincter (nitrates and nifedipine). However, the relatively high frequency of side effects (peripheral edema, headache, and hypotension) and the lack of controlled studies limit their use to patients with early-stage disease, as a temporary measure before a longer option is available. definitive is chosen [8,9].
Botulinum neurotoxins (abbreviated BoTx A through G) cause prolonged inhibition of neurotransmitter release at cholinergic terminals. Published studies have reported that after a single injection of the toxin, nearly 80% of patients report good to excellent symptom relief. More than half are still in remission at six months and a third at one year [10]. Forced dilation of the lower esophageal sphincter under fluoroscopic guidance in the supine position is considered the most effective non-surgical treatment for achalasia.
The safest and most effective treatment for achalasia is surgery, which involves cutting the muscle fibers of the abnormally functioning lower esophageal sphincter (a Heller cardiomyotomy). Minimally invasive (laparoscopic and thoracoscopic) types of Heller myotomy were introduced into clinical practice in the early 1990 [1]. To reduce the risk of Gastroesophageal Reflux Disease (GERD) following cardiomyotomy, which until then had been used alone, the operation was then supplemented by partial fundoplication (anterior-Dor, or posterior-Toupet). This modified laparoscopic Heller's cardiomyotomy supplemented with semifundoplication has proven to be the most effective procedure, with minimal morbidity, both short and long term [1,11]. Heller's cardiomyotomy by laparotomy was the only therapeutic option available and performed in our case. She was associated with a Toupet-type fundoplication.
Achalasia is a chronic esophageal motility disorder characterized by the inability of the lower esophageal sphincter to relax. Heller's cardiomyotomy by laparotomy associated with Toupet-type fundoplication still retains its place in the management of esophageal achalasia in our exercise context.
We have no known conflict of interest to disclose.
No
