 Journal of Medical Research and Surgery
PROVIDES A UNIQUE PLATFORM TO PUBLISH ORIGINAL RESEARCH AND REMODEL THE KNOWLEDGE IN THE AREA OF MEDICAL AND SURGERY
Journal of Medical Research and Surgery
PROVIDES A UNIQUE PLATFORM TO PUBLISH ORIGINAL RESEARCH AND REMODEL THE KNOWLEDGE IN THE AREA OF MEDICAL AND SURGERY
 Journal of Medical Research and Surgery
PROVIDES A UNIQUE PLATFORM TO PUBLISH ORIGINAL RESEARCH AND REMODEL THE KNOWLEDGE IN THE AREA OF MEDICAL AND SURGERY
Journal of Medical Research and Surgery
PROVIDES A UNIQUE PLATFORM TO PUBLISH ORIGINAL RESEARCH AND REMODEL THE KNOWLEDGE IN THE AREA OF MEDICAL AND SURGERY
 Indexed Articles
Indexed ArticlesSelect your language of interest to view the total content in your interested language
Ninad Godghate1* , Neha Godghate1, Tim Drew2, Krishnamohan Saindane3
, Neha Godghate1, Tim Drew2, Krishnamohan Saindane3
1Director, Grace Orthocare and Multispeciality Hospital, Nagpur, Maharashtra, India
2Senior Lecturer, Department of Orthopaedic and Trauma Surgery, Ninewells Hospital, University of Dundee, Scotland
3Director, Suyog Hospital, Dhule, Maharashtra, India
Correspondence to: Ninad Godghate, Director, Grace Orthocare and Multispeciality Hospital, Nagpur, Maharashtra, India
Received date: November 22, 2022; Accepted date: December 13, 2022; Published date: December 20, 2022
Citation: Godghate N, Godghate N, Drew T, et al. A Simple Device to Determine Ante-Version During Femoral Prosthesis Insertion in Total Hip Replacement. J Med Res Surg. 2022; 3(6): 119-122. doi: 10.52916/jmrs224093
Copyright: ©2022 Godghate N, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted
use, distribution and reproduction in any medium, provided the original author and source are credited.
Introduction: Good outcomes in Total Hip Replacement (THR) depend upon correct component alignment. This is influenced by the surgeon’s capacity to recreate a geometrically normal and biomechanically stable hip joint. Mal-positioining of components can lead to various complications and the surgeons have to make vital decisions intra-operatively based on their experience. Materials and Methods: This study describes a simple instrument to aid alignment of femoral stem insertion and hence achieve the normal range of ante-version between 10 º-20 º. Experiments performed on a saw bone model by twenty orthopaedic surgeons, each making six attempts to insert a prosthesis demonstrated improved positioning when compared to unaided insertion. Results: The mean average femoral stem ante-version unaided was 18.3 º (range, 4.9 º to 36.6 º). Device aided ante-version was 14.4 º (range, 9.8 º to 18.9 º) (p<0.001). We also report the practicality of the use of the device which was assessed by use on cadavers. Conclusion: Precise assessment of stem ante-version can be achieved in non-navigated THR if such a device is available intra-operatively.
Total hip replacement, Femoral stem ante-version, Intra-operative alignment device, Prosthesis, Implementation
Survival outcomes of Total Hip Replacement (THR) are influenced by the capacity of the surgeon to recreate a geometrically normal and biomechanically stable hip joint with appropriate implants in a thoroughly assessed patient. Scrupulous attention to detail and a strict implementation of proper surgical technique is necessary to avoid complications including impingement, dislocation and infection. A well performed surgery has been shown to provide long lasting benefits and functionally improve the quality of life of the patients. However, associated complications can be present in about 5%-10% of cases, almost half of which can be attributed to incorrect placement of implants [1]. This number can significantly increase in technically demanding surgeries. The mal-positioning of one or both components can cause dislocation, impingement, wear and aseptic loosening [2]. The importance of achieving an accurate position of both the acetabular as well as the femoral components has been stressed by many studies [3-5]. However the use of intra-operative devices that will guide the surgeon in inserting the femoral stem in the desired amount of ante-version is little reported. Although computer navigation can enhance surgical precision, this functionality has not been used widely, mostly due to financial constraints [6]. In most cases, the surgeon has to rely on judgment and experience, but the increasing incidence of post-surgical instability raises the question as to whether the required goals are being widely achieved [7]. Our study aims to address a part of this problem by introducing the use of a new device that improves femoral ante-version positioning.
A prototype positioning device was manufactured (Figure 1A). It consisted of a Lowman’s clamp, an angular scale with a radius of five centimeters and two holes positioned at zero and fifteen degrees respectively, to accommodate an alignment pin measuring five centimeters in length. The angular scale was attached to a Lowman’s clamp via link joints in a manner allowing independent translation of the scale along three orthogonal axes, but constraining rotation about the X and Y axes. A slot with a locking screw at one end of the goniometer allowed anteroposterior movement (translation along the Z axis) while two flexible links allowed movement in the mediolateral and supero-inferior directions (translation along the X and Y axes). An experimental model of the femur was developed to evaluate the device. This consisted of a saw-bone model of a left lower limb attached to a table. The tibia was kept in a constant vertical position and perpendicular to the longitudinal axis of the femur. This is the same position adopted whilst performing THR surgery through a posterior approach. The femoral neck was osteotomised one centimeter above the lesser trochanter and the canal widened with a reamer. A digital camera attached to a tripod stand was aligned with the longitudinal axis of the femur (Figure 1B). This was positioned using a straight rod to align the femoral canal with the lens of the camera. The position of the stand and the tripod were marked on the lab floor with a marker pen, to ensure consistent alignment throughout the experiments. A polished collar-less CPT stem was used for insertion in the femur. A play-dough-style substance was used to simulate poly-methyl methacrylate cement.
With the Lowman’s clamp applied to the femur below the lesser trochanter and the guide pin placed in the zero degree hole, the goniometer was moved to align the pointed end of the guide pin centrally in the medullary canal. After achieving a satisfactory alignment, the position of the goniometer was maintained and the guide pin was removed and partially inserted in the fifteen-degree hole which acted as a reference for the final stem insertion.
Photographs of the inserted stem were taken after each attempt and the angular position of the stem was measured using CAD software. The reference lines used for measurement were a straight vertical line from the center of the stem and a line through the center of the neck of the stem. The ante-version angle of the stem was calculated by subtracting ninety degrees from this angle. The precision of this measurement technique was established by taking images of a circular sheet with known angles drawn on it, the center of which was aligned to the longitudinal axis of the femur.
Twenty orthopaedic surgeons with an average clinical experience of five years were selected for the experimental evaluation of the device. All surgeons were familiar with the posterior approach to the hip and practiced the visual assessment technique for femoral stem anteversion. Each surgeon was asked to insert the femoral stem manually in the saw bone model in fifteen degrees of anteversion without changing the position of the assembly. Six attempts, three with and three without the device were given to each surgeon and the application of the device was demonstrated before the experiment individually. Photographs were taken after each attempt and transferred to the computer for measurement.
A total of 120 values were available after the experiment. Sixty values were from the group without using the device and labeled as Visual Estimation (VE). Sixty values were from the group using the device and labeled as Device Assisted (DA). Results were analyzed using the Statistical Package for Social Sciences version 17 (SPSS). The mean, the range, the maximum and minimum values (Figure 2A), and the standard deviation were calculated for each group (Table 1). Statistical comparisons were performed by using the paired t-test. A p-value less than 0.05 was considered statistically significant. Accurate insertion was defined as an angle measured within three degrees of the reference angle of 15 degrees (15 ± 3). In the VE group 58.34% of the values were lying beyond 5 degrees (<10 or >20) of the reference angle of 15 degrees of which 11.66% were less than 10 degrees and 46.66% were more than 20 degrees.
Visual estimation |
Device assisted |
|
| Minimum value | 4.97 ° |
9.83 ° |
| Maximum value | 38.66 ° |
18.92 ° |
| Average ante-version | 18.32 ° |
14.41 ° |
| Standard deviation | 7.13 |
1.76 |
This showed that when errors occur, surgeons tend to insert the stem in excessive anteversion most of the time. With the use of the device, 90% of the values were accurate and 98.33% were within four degrees of the reference angle. Angles measured without the device showed that 8.33% were within one degree, 16.66% were within two degrees, 28.33% were within three degrees and 38.33% were within four degrees of the reference angle of 15 degrees. Angles measured with the device showed that 48.33% were within one degree, 73.33% within two degrees, 90% within three degrees and 98.33% within four degrees of the reference angle of 15 degrees (Figure 2B). Comparison of the two groups using the paired t-test showed significant difference (p value <0.001). The average value without the device was better than with the device in the two subjects with a difference of 0.7 degrees in both cases.
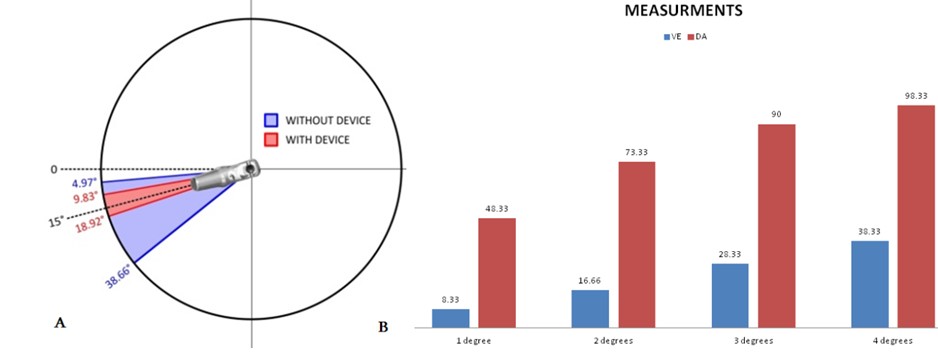 Figure 2: (A) Range of ante-version with and without the device; (B) Comparative accuracy in two groups.
Figure 2: (A) Range of ante-version with and without the device; (B) Comparative accuracy in two groups.Results showed that in the group without the device 58.34% of the values were beyond five degrees (>20 or <10) of the reference angle of 15 degrees. Dorr, et al. [8] compared surgeon estimation and computed tomography measurement of femoral stem anteversion in 109 cement-less THRs and found that 55% were outside the desired range of 10 to 20 degrees. Wines and McNicol [9] used two-dimensional computed tomographic scans for measurement of stem anteversion (cemented and uncemented) in 111 hips and reported that only 30% achieved a range of 10 degrees to 20 degrees of ante-version. Sendtner, et al. [10] evaluated stem ante-version in 60 patients and found that the prevalence of abnormal stem ante-version was 92%. These values demonstrate that errors in visual estimation can be significant and that mere judgment using one or two planes is insufficient. Furthermore, the errors can be cumulative if the placement of the acetabular cup is also incorrect. If the stem ante-version is abnormal, the acetabular safe zone of 15 degrees to 20 degrees does not give an acceptable combined ante- version which is an important measure of the stability of THR.
The current surgical technique results in significant variation between the anatomical and the surgically reconstructed femoral ante-version. One possible reason for the variability in ante- version could be the limited availability of osseous landmarks. Once the femoral neck is cut, any hints about the accurate degree of ante-version of that particular hip are lost and only general guidelines can be applied. The normal anteversion begins at the level of the lesser trochanter, continues through the inter-trochanteric region, and is completed in the ante-version of the neck. In THR it is defined as the angle between the transcondylar plane and a plane including the axis of the femoral shaft and the neck of the femoral component [11]. The true neck axis is defined as a line passing through the midpoints of the neck at the most proximal portion of the inferior neck with no head portion while the level of the neck osteotomy intra-operatively is about one centimeter proximal to the lesser trochanter [12]. Other factors controlling stem ante-version are the width of the medullary canal, the thickness of the posterior cortex, and the anterolateral bowing of the femur. Dorr, et al. [8] found that the stem anteversion increased in the osteoporotic bone while thicker bones forced the stem posteriorly in metaphysis which increased retroversion.
Further compounding factors are variations in ante-version which can be present between males and females, right and left side; and a normal and pathological hip. Surgeons who operate with the patient in the supine position may visualize the femur and the cup in a different plane and Maini, et al. [13] found that the operating surgeon had better control over the femoral anteversion through the posterior approach when compared to the anterior approach. The femoral stem has to be implanted in line with the proximal femoral axis avoiding any tilt in the frontal and sagittal plane. Müller, et al. [2] investigated the influence of stem tilting in the sagittal plane on the position of the center of the femoral head and also on prosthesis torsion. It was observed that a tilt of two degrees either anteriorly or posteriorly changes the anteversion by five degrees. Thus if a stem implanted in 15 degrees of ante-version is tilted anteriorly by two degrees the functional ante-version becomes 20 degrees instead of 15 degrees. The rotatory anteversion intended by the surgeon may be functionally significantly different. Since the femoral stem is placed in a closed canal, it is difficult for the surgeon to sufficiently evaluate the proximal femoral axis during surgery. In such an instance, gross errors can be avoided if the stem ante-version is within the normal range. As the hip joint is a major load-bearing structure, implants used in THR have to sustain cyclical loads for many years. Apart from body weight and activities, load distribution on the hip joint can be influenced by implant material, fixation, and orientation. Incorrect placement of implants significantly increases forces acting on a joint surface which leads to wear and shortens the life of the prosthesis. Mirghaderi, et al. [14] have shown that pre-operative templating can improve efficiency of the surgical process by predicting implant position and alignment. However, due to lack of useful guides intra-operatively, it can be difficult to ascertain if the ideal position has been achieved succesfully.
Although promising results were seen with the use of the device, there are some limitations of this study. The femoral ante-version is defined in three dimensions, but the measurement technique used in the study was two dimensional and therefore final comments on the actual precision of the device can only be made after in-vivo studies. Another limitation is the subjective variation that can be present while applying the device parallel to the tibia and locating the alignment pin centrally in the medullary canal. Difficulties in using the device may also be encountered because present surgical exposure restricts the use of such bulky instruments. These shortcomings were addressed in a modified version in which a smaller assembly was mounted over a Schanz pin that could be inserted in the lesser trochanter aided by a specially designed drill sleeve and by providing a small circle at the end point of the alignment pin which can be positioned over the medullary canal. This modified version was tested on a saw bone model (Figure 3A) and found to be equally effective. To explore its intra-operative application a cadaver study was performed and it was observed that the device could be applied through a posterior approach without much difficulty (Figure 3B).
A wide variability in the values from the two groups in our study is in agreement with findings from other studies that have compared surgical accuracy to computer navigation. These findings make a persuasive case for the development of instruments that can reliably and accurately improve surgical performance and provide a cheaper alternative to the enormous cost required in computer navigation. The improved values in the group using the device strongly support the viability of the instrument. This suggests that if such a device is available intra-operatively the surgeon will be able to reliably insert the femoral stem in the targeted normal range of 10-20 degrees. Achieving this normal range can be comparatively easier in the case of cemented THR due to the rotational freedom which is restricted in the case of un-cemented THR. However, it could also be useful to have such a device even in un-cemented THR as the surgeon would have an estimate of the stem anteversion and could use this knowledge to change the anteversion of the cup to achieve a normally combined anteversion. Considering the significant rise in the number of primary and revision surgeries measures need to be taken for prolonging the life of implants especially in younger populations. Such interventions to ensure that primary surgeries are successful will not only reduce the financial burden on the health care community but also lessen the risks associated with revision surgery.
Computer navigation-assisted surgeries have been shown to improve the success of joint replacement by allowing more accurate and precise implant alignment. It decreases the variability with regard to component orientation by providing the surgeon with immediate intra-operative feedback with regard to the actual position of the component and overcomes any deficiencies in the three-dimensional vision. However, computer navigation in THR is not very common as the broader application of this system is still hindered by increased operative times, partly due to the complexity of the system. The accompanying financial costs are also considerable. Other obstacles are bulky equipment in the operating room, additional navigation steps throughout the procedure, and a learning curve to master the technique. It is reasonable to speculate at this juncture that a simple device, perhaps similar to our prototype, may overcome the limitations of computer navigation by providing a reliable, inexpensive, and effective solution to deal with component alignment in THR. Further studies are needed to establish the clinical practicality and usefulness of the device and any definitive conclusions about the actual efficacy of the device can only be made after using it in vivo and precise measurements carried out with Computed Tomography (CT) scans before and after surgery.
The author declare no competing financial interest.
No.
