 Journal of Medical Research and Surgery
PROVIDES A UNIQUE PLATFORM TO PUBLISH ORIGINAL RESEARCH AND REMODEL THE KNOWLEDGE IN THE AREA OF MEDICAL AND SURGERY
Journal of Medical Research and Surgery
PROVIDES A UNIQUE PLATFORM TO PUBLISH ORIGINAL RESEARCH AND REMODEL THE KNOWLEDGE IN THE AREA OF MEDICAL AND SURGERY
 Journal of Medical Research and Surgery
PROVIDES A UNIQUE PLATFORM TO PUBLISH ORIGINAL RESEARCH AND REMODEL THE KNOWLEDGE IN THE AREA OF MEDICAL AND SURGERY
Journal of Medical Research and Surgery
PROVIDES A UNIQUE PLATFORM TO PUBLISH ORIGINAL RESEARCH AND REMODEL THE KNOWLEDGE IN THE AREA OF MEDICAL AND SURGERY
 Indexed Articles
Indexed ArticlesSelect your language of interest to view the total content in your interested language
Yasrab Ismail1,2* , Sanobar Bughio1
, Sanobar Bughio1
1Consultant Radiologist, Dr Ziauddin Hospital, Karachi, Pakistan.
2Consultant Radiologist Craigavon Area Hospital, Northern Ireland, United Kingdom.
Correspondence to: Yasrab Ismail, Consultant Radiologist, Dr Ziauddin Hospital, Karachi, Pakistan.
Received date: February 16, 2024; Accepted date: March 07, 2024; Published date: March 14, 2024
Citation: Ismail Y, Bughio S. A Rare Complication of Percutaneous Endoscopic Gastrostomy Tube Placement: Early Buried Bumper Syndrome (BBS). J Med Res Surg. 2024;5(1):22-24. doi: 10.52916/jmrs244131
Copyright: ©2024 Ismail Y, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted
use, distribution and reproduction in any medium, provided the original author and source are credited.
Early Buried Bumper Syndrome (BBS) is a rare complication of Percutaneous Endoscopic Gastrostomy (PEG) tube placement where the internal bolster gets “buried” in the gastrocutaneous fistulous tract. BBS is usually a late complication. We present a case of early BBS, in Radiology Department of Dr Ziauddin Hospital, Karachi. Patient presented with fever and oozing from the side of PEG tube. CT scan abdomen findings revealed, the bumper of the percutaneous endoscopic gastrostomy tube retracted in subcutaneous fat just adjacent to the gastric wall and seen in the left sided rectus sheath outside the gastric lumen. Contrast was given through the peg during the procedure which show no extravasation of contrast in adjacent soft tissues. These findings consistent with early buried bumper syndrome.
Buried Bumper Syndrome (BBS), Percutaneous Endoscopic Gastrostomy (PEG, Esophagus cancer, CT scan, Gastrointestinal.
Gauderer and Ponsky, who primary introduce the percutaneous endoscopic gastrostomy (PEG). in 1980. Dr. Michael W. Gauderer and Dr. Jeffrey L. Ponsky played pivotal roles in the development and refinement of PEG, revolutionizing the way enteral access is provided to patients who are unable to consume food, water, or medication orally [1]. The PEG procedure involves the placement of a feeding tube directly into the stomach through the abdominal wall, allowing for the administration of nutrition and medications. This technique has become a standard and widely used method for long-term enteral feeding in individuals who cannot adequately swallow or take oral nutrition, it has significantly improved the management of patients with various medical conditions, including those with neurological disorders, head and neck cancers, and other conditions that compromise their ability to ingest food orally [1].
The use of PEG tube placement is generally considered a safe and effective method for providing long-term enteral nutrition to patients who are unable to take foods, water, and medication by mouth. While complications are relatively rare, it's important to be aware of potential risks associated with the procedure, such as bleeding, infection, leakage, peritonitis, necrotizing fasciitis, tumor seeding, ileus, and Buried Bumper Syndrome (BBS) [2-4]. The overall success rate of this procedure is 94% to 98%, which is significantly better than that of fluoroscopic procedures. There are various factors that can prevent successful placement, such as obstruction of pharynx or esophagus, in addition poor transillumination of wall and the development of a hematoma. Other factors such as prior surgery can also affect the quality of the procedure. For instance, alterations to the gastric or esophagus anatomy can lead to difficult and invasive PEG placement [6].
We present here a case of BBS followed by a discussion of its etiology, management, and prevention.
The 84-year-old woman, who was a k/c of HTN, had been diagnosed with esophagus cancer. Later on a PEG tube was placed as a part of palliative care. She had presented with fever and blood oozing from the side of the PEG tube. She was then sent to the radiology department for evaluation of the position of the tube in department of CT scan abdomen with contrast for evaluation of PEG tube position.
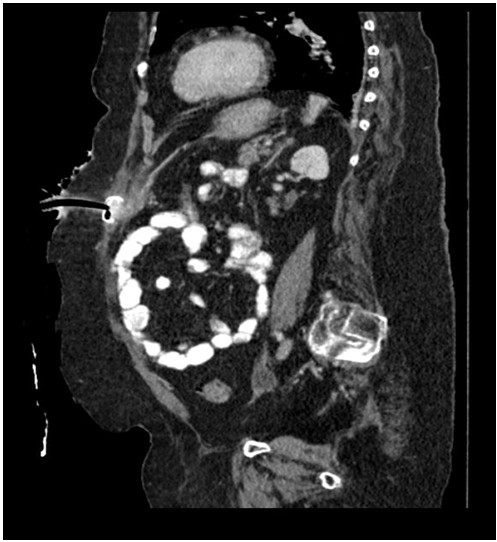 Figure 1: Sagittal post contrast image, showing the abnormal subcutaneous malposition of bumper of peg tube.
Figure 1: Sagittal post contrast image, showing the abnormal subcutaneous malposition of bumper of peg tube.CT scan abdomen findings revealed, the bumper of the percutaneous endoscopic gastrostomy tube retracted in subcutaneous fat just adjacent to the gastric wall and seen in the left sided rectus sheath outside the gastric lumen. Contrast was given through the peg during the procedure which show no extravasation of contrast in adjacent soft tissues. These findings consistent of early buried bumper syndrome (Figure 1,2).
Figure 1 and 2 describes the CT scan of the abdomen with contrast sagittal and axial image showsretraction of the internal bumper of the percutaneous endoscopic gastrostomy tube (solid white arrow) into the subcutaneous fat adjacent to the gastric wall.
Gauderer and Ponsky, who primary introduce the Percutaneous Endoscopic Gastrostomy (PEG). In 1980, Dr. Michael W. Gauderer and Dr. Jeffrey L. Ponsky played pivotal roles in the development and refinement of PEG, revolutionizing the way enteral access is provided to patients who are unable to consume food, water, or medication orally [1]. Percutaneous Endoscopic Gastrostomy (PEG) tubes are indeed indicated for a variety of medical conditions, especially those affecting the ability to eat or swallow such as Neurological disorders, head and neck cancers, severe malnutrition esophageal disorders, trauma or surgery, prolonged coma or unconsciousness chronic diseases [7]. The use of PEG tube placement is generally considered a safe and effective method for providing long-term enteral nutrition to patients who are unable to take foods, water, and medication by mouth. It has rare and often late complication of the use of PEG tube. In some cases, it may manifest as early as three weeks after the PEG tube placement which occurs when the internal bumper migrates through the gastric wall. Associated with varying type co-morbidities [8].
The decision to place a PEG tube is made based on a thorough assessment of the patient's medical condition, nutritional status, and the likelihood of recovery or improvement in oral intake. It is an important intervention to ensure that individuals receive the necessary nutrients when oral intake is compromised, helping to improve overall health and quality of life [8].
The average lifespan of a percutaneous endoscopic gastrostomy (PEG) tube is typically one to two years, although individual cases may vary. Tube replacement may become necessary due to complications such as Buried Bumper Syndrome (BBS), which can occur when the internal bumper of the PEG tube becomes embedded in the gastric wall [9].
It is crucial for healthcare professionals to assess the specific situation, considering factors such as the severity of BBS, the patient's overall health, and the presence of complications when deciding on the appropriate approach for PEG tube replacement. Regular follow-up and surveillance of PEG tube sites are essential to detect any signs of complications and ensure timely intervention.
Since its introduction in 1980, Percutaneous Endoscopic Gastrostomy (PEG) has indeed gained worldwide acceptance as a safe and effective technique for providing enteral feeding in patients with poor oral intake who have a functional Gastrointestinal (GI) system. PEG tube placement is recommended for a variety of indications, especially when oral feeding is not possible or sufficient.
BBS is a rare and often late complication of the use of PEG tube. In some cases, it may manifest as early as three weeks after the PEG tube placement. BBS occurs when the internal bumper of the feeding tube becomes embedded in the gastric or abdominal wall, making removal or repositioning of the tube difficult. Characterized by the migration of the internal bumper into the gastric or abdominal wall tissue, leading to symptoms such as pain, leakage around the tube site, and difficulty or inability to aspirate gastric contents. It is considered a rare but serious complication that requires prompt attention and intervention.
Early recognition of BBS is very important in order to minimize its life-threatening consequences. A multidisciplinary approach is needed to prevent it.
The authors of the paper you are referring to have declared no conflicts of interest or financial gain.
No.
