 Journal of Clinical and Biomedical Investigation
PROVIDES A UNIQUE PLATFORM COVERING SCIENTIFIC KNOWLEDGE IN BIOMEDICAL SCIENCES AND CLINICAL RESEARCH
Journal of Clinical and Biomedical Investigation
PROVIDES A UNIQUE PLATFORM COVERING SCIENTIFIC KNOWLEDGE IN BIOMEDICAL SCIENCES AND CLINICAL RESEARCH
 Journal of Clinical and Biomedical Investigation
PROVIDES A UNIQUE PLATFORM COVERING SCIENTIFIC KNOWLEDGE IN BIOMEDICAL SCIENCES AND CLINICAL RESEARCH
Journal of Clinical and Biomedical Investigation
PROVIDES A UNIQUE PLATFORM COVERING SCIENTIFIC KNOWLEDGE IN BIOMEDICAL SCIENCES AND CLINICAL RESEARCH
Aliya Ishaq1*, Muhammad Shadab Khan2, Mariya Ishaq3, Ayesha Saba4, Turab Pishori5
1Specialist General and Minimal Acess Surgeon in Dubai Hospital, Associate Professor Dubai Medical College, Dubai
2Assistant Professor, Sindh Institute of Urology and Transplantation Karachi, Pakistan
3Medical Officer Sindh Children Services Hoapital Karachi, Pakistan
4Consultant Gyanecologist Indus Hospital Karachi, Pakistan
5Professor of Surgery at Portland Hospital State of Victoria, Australia
Correspondence to: Aliya Ishaq ,Specialist General and Minimal Acess Surgeon in Dubai Hospital ,Associate Professor Dubai Medical College, Dubai Uae, Email: aishaq@dha.gov.ae/draliya_ishaq@yahoo.oom
Received date: May 29 , 2021; Accepted date: June 15, 2021; Published date: June 22, 2021
Citation: Ishaq A, Khan MS, Ishaq M, et al. (2021) Ilioinguinal Neurectomy and Chronic Post-Operative Pain After Inguinal Hernia Repair. J Clin Biomed Invest 1(1): pp. 1-7. doi: 10.52916/jcbi214005
Copyright: ©2021 Ishaq A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Objective: This study aims to determine the effect of preservation /division of ilioinguinal nerve in patients undergoing lichenstein hernioraphy on severity of chronic post operative pain as well well as presence /absence of groin numbness.
Method: A randamised control trial was conducted for a period of six months on 60 patient fulfilling inclusion criteria who underwent lichenstein hernioraphy at general surgery department of Liaquat National university hospital Karachi , Pakistan.
Result: A total of 60 patients undergoing elective inguinal hernia mesh repair were Included in study and divided in two groups with 30 patients each. Only male patients were included in the study as female gender was one of the exclusion criteria so gender stratification was no considered. Patients between 17 to 77 yrs of age were included in study and randomly divided in two groups. Mean age of population in group A is 42.96 +/- 17.76 an in group B is 54.23 +/- 15.0. The minimum age of the patient in Group A is 17 years and maximum age is 73 years whereas minimum age of the patient in Group B is 20 years and maximum age is 77 years.
Chronic groin pain while different physical activities and groin numbness in nerve preservation and nerve division group was assessed at three and six months follow ups in all patients of the study population. 3% of the patients from nerve preservation group had mild pain during climbing stairs at three and six months follow up and the P-Value was 0.313 which is statistically not significant. 10% of the patients from nerve division group and 50% patients from nerve preservation group had pain during brisk walking at three months follow up and the P-Value was 0.001 which is statistically significant. 23% of the patients from nerve division group and 60% patients from nerve preservation group had pain during brisk walking at six months follow up and the P-Value was 0.004 which is statistically significant. 13.3% patients from nerve preservation group had moderate pain during brisk walking at three months follow up while none of the patient from nerve division group had pain and P-Value was 0.038 which is statistically significant. 6.6% of the patients from nerve preservation group had moderate pain during brisk walking at six months follow up while none of the patient from nerve division group had pain and p-value was 0.150 which is statistically in significant. 20% of the patients from nerve division group and 30% of the patients from nerve preservation group had mild groin numbness at three months follow up with P-Value of 0.371 which is statistically in significant. 33.3% of the patients from nerve division group and 30% of the patients from nerve preservation group had groin numbness at six months follow up with a p-value of 0.781 which is statistically in significant.
Conclusion: Prophylactic ilioinguinal neurectomy during Lichtenstein tension free inguinal hernia repair decreases the incidence of exertional chronic post operative pain as compare to the nerve preservation group. However the cutaneous neurosensory disturbance/groin numbness between the two groups has no difference in term of outcome.
In order to prepare ourselves from a expected third wave of Covid-19, we should not repeat mistakes that we made during previos waves. We should refrain ourselves from dismantling our enhanced healthcare facilities, there should not be any sorts of shortage of oxygen , hospital beds, and drug that we have already witnessed. We must have an aggressive containment measure comprising of a really strong and pro-active surveillance system. This can be achieved by increasing the capacity of the existing surveillance system by identifying active cases early. We must ensure that we should follow “social vaccine” of proper masking, avoid indoor gatherings, and proper sanitization. Our vaccination programme needs a boost. We should vaccinate a large section of people before any third wave hits us. The more we vaccinate, the better prepared we are. As medical professionals, it must be ensured that proper scientific protocol must be implemented while handling Covid-19 cases. And last but not the least efforts must be made to fill up vacancies seen in our public health system, especially for frontline healthcare workers.
As it is anticipated that the young children are more vulnerable to the forthcoming third wave, efforts are to be sought in order to start vaccination of the younger children in our country. Trials for which has already been started in India and across the world. Till the time vaccine is made available, the resources are to be mobilized to build up healthcare facilities catering the vulnerable age group in this third wave such as building up of more paediatric wards, paediatric ICU’s , training of healthcare personals in handling the emergencies for expected third wave .In addition to these efforts , more and more paediatric covid care centers must be set up at various parts of the country. Equally important is making arrangements for rehabilitation centers for the orphans. Countries like US, Singapore and UAE have already started vaccinating the children in age group between 12 to 15 years with Pfizer-BioNTech Covid vaccine. It’s a high time that the government in India must consider for allowing “expedited approval pathway” to the companies like Pfizer for their Covid-19 vaccine for children. All these combined efforts from everyone may ensure that the country and world may remain well equipped against these subsequent waves of this deadly virus and pave the path of the triumph in the near future.
Ileoinguinal hernia is the most common male disease worldwide [1] . Repair of inguinal hernia is the second most commonly performed general surgery procedure [1-4]. The most annoying complication is chronic post-operative pain causes include trauma during dissection to ilioinguinal nerve passing through the surgical field, fibrosis and inflammation induced by the prosthetic mesh in close proximity to ilioinguinal nerve, strangulation of the nerve caught by suturing etc. [1-3]. Chronic post-operative pain has been reported in 19% to 69% cases of inguinal hernia repair. Severe groin pain has been reported in 3% cases [1-3]. Chronic pain has been reported as the pain that lasts longer than the usual healing time of six weeks. Various time scales have been suggested, usually 3 or 6 months [1]. The ilioinguinal nerve encountered during open repair of the inguinal hernia as it lies immediately beneath the external oblique aponeurosis .Tradionally the nerve is preserved during repair because of the expected cutaneous sensory loss and chronic groin pain following nerve injury [2-3].
Studies on ilioinguinal neurectomy during hernia repair have shown decrease in the incidence of chronic groin pain compare to the routine nerve preservation [1]. However the results have been inconsistent. The control trials by Picchio et al found similar incidence of loss of pain sensation between ilioinguinal nerve preservation versus division group i.e. 5% Vs 33% at six months where P-value is statically not significant. However the incidence of loss of touch sensation between the two groups is 6% Vs 29% at six months where the P-value is statically significant. It concludes that elective division of the ilioinguinal nerve negatively affects the groin numbness while it has no effects on chronic groin pain. On the other hand control trails by Dittrick et al. [2] concludes that the incidence of chronic groin pain between nerve excisions versus preservation group is 3% Vs 26% at six months where P-value is statically significant. However the incidence of groin numbness between the two groups is 18% Vs 4% at six months where P-value is statically not significant. It concludes that elective division of ilioinguinal nerve reduces post operative groin pain and has no effect on groin numbness.
The aim of this study is to assess the effect of preservation or the division of ilioinguinal nerve on post operative groin pain and numbness after open inguinal hernia repair with polyprolene mesh. The results will help to reduce troublesome complication of open inguinal hernia repair.
To determine the effect of preservation versus division of ilioinguinal nerve in patients under going inguinal hernia mesh repair on,
Pain that lasts longer than three months duration. Clinically neuropathic pain is typically characterized as a burning or shooting pain in the distribution of the effected nerve. Severityof the pain will be calculated using Visual Analog Score.
A visual analog score is a useful device for accurately determining the level of pain. The patient indicates the intensity of pain he/ she is feeling as mild (1-3), moderate (4-7) and severe (8-10) [2].
Change in the level of sensation along the distribution of ilioinguinal nerve i.e skin over the groin region specially medial aspect of thigh, the upper part of scortum and the penile root compared to the non operative healthy side. Technique of evaluation include needle point prick for pain and wisp of cotton for touch. Post operative presence and absence of numbness will be evaluated at three and six month.
Prophylactic ilioinguinal neurectomy significantly decreases the incidence of chronic groin pain after inguinal hernia mesh repair and has no effect on the post operative groin numbness.
Department of General Surgery, Liaquat National Hospital Karachi.
Six months.
P1= 3%, P2= 26%
1-beta= 80%, 1- alpha= 95%
N=60, (n1= 30 patients group A, n2= 30 patients group B)
Non probability purposive sampling.
Randomized control trials.
After selecting patients according to inclusion and exclusion criteria, patient will be informed about the study and its purpose. Verbal and written consent will be taken from the patients. Patients will be included in study only if they give will consent and approval from the ethical committee of LNH has been taken. Demographic details will be taken from case file as well as directly interviewing the patient. Data will be filled by principle investigator on the performa attached at the end. Patients selected for the elective hernia repair undergo standard tension free herniorraphy. Standard tension free herniorraphy involves placement of an approximately 11cm × 6 cm ( tailored to the individual patient requirements) mesh as an extra lamina anterior to the posterior wall and overlapping it generously in all directions including medially over the pubic tubercle . After identification of the ilioinguinal nerve during surgery a slip will be taken randomly from the box, already containing equal number of marked slips with group A/B.
This will be done per operatively (when patient is under anesthesia) because sometime ilioinguinal nerve is not identified and such patient will be excluded from study
Patient will be followed by the primary investigator who will not be involved in randomization process. All patients will receive the standard mesh repair procedure and will be managed in a standard clinical pathway post operatively and will be followed at three and six month in OPD (Final out come will be measured at six month). The researcher will keep a log of all patients included in the study and will take their contact numbers and will communicate with other team members so that he can be called once the patient came in OPD and in case of non arrival on the expected visits patients will be contacted by calling them on contact numbers.
Primary outcome measured will be the occurrence of chronic groin pain at six months after surgery.
On the follow up visit the presence and severity of postoperative pain after following activities will be inquired from the patients.
VAS with total 10 points (1-10) will be used to determine the severity of pain as Non(0), Mild (1-3), Moderate (4-7) and Severe (8-10).
Post-operative presence or absence of groin numbness in each patient will be assessed and documented on their OPD follow ups visits at six month while comparing with the opposite non operative side.
An approval from hospital ethical committee has been taken. Patient/ attendant explained regarding whole procedure and there written and verbal consent taken. Further details have been mentioned in consent form attached. No external source of funding was required and sought. There is no conflict of interest in any of the two groups of study.
A total of 60 patients under going elective inguinal hernia mesh repair included 30 patients in each group. None of the patients lost to follow up so all 60 patients were included in the study, as shown in Table 1.
| Group | Frequency | Percentage |
| Nerve preservation | 30 | 50.0 |
| Nerve division | 30 | 50.0 |
| Total | 60 | 100 |
Out of 60 Patients included in the study population, patients divided according to the site of hernia operated (Table 2).
| Site | Frequency | Percentage |
| Left | 23 | 38.3 % |
| Right | 37 | 61.7 % |
| Total | 60 | 100 % |
45.9% Patients in group A (Nerve preservation group) have right inguinal hernia.
54.0% Patients in group B (Nerve Division group) have right inguinal hernia.
56.5% Patients in group A (Nerve Preservation group) have left inguinal hernia.
43.4% Patients in group B (Nerve Division group) have left inguinal hernia.
Only male patients were included in the study as female gender was one of the exclusion criteria so gender stratification was no considered.
Patients between 17 to 77 yrs of age were included in study and randomly divided in two groups. Mean age of population in group A is 42.96 +/- 17.76 an in group B is 54.23 +/- 15.0. The minimum age of the patient in Group A is 17 years and maximum age is 73 years whereas minimum age of the patient in Group B is 20 years and maximum age is 77 years (Table 3).| Site | Nerve preservation | Nerve division |
| Left | 13 | 10 |
| Right | 17 | 20 |
| Total | 30 | 30 |
Chronic groin pain while different physical activities and groin numbness in nerve preservation and nerve division group was assessed at three and six months follow ups in all patients of the study population.
Mild chronic groin pain during rest at three months follow up was observed in both nerve preservation and nerve dissection group and in both groups no change noticed because both groups have no pain.
Mild chronic groin pain during rest at six months follow up was observed in both nerve preservation and nerve dissection group and in both groups no change noticed because both groups have no pain.
Moderate chronic groin pain during rest at three months follow up was observed in both nerve preservation and nerve dissection group and in both groups no change noticed because both groups have no pain.
Moderate chronic groin pain during rest at six months follow up was observed in both nerve preservation and nerve dissection group and in both groups no change noticed because both groups have no pain.
Severe chronic groin pain at rest at three months follow up was observed in both nerve preservation and nerve dissection group and in both groups no change noticed because both groups have no pain.
Severe chronic groin pain at rest at six months follow up was observed in both nerve preservation and nerve dissection group and in both groups no change noticed because both groups have no pain.
Mild chronic groin pain during coughing at three months follow up in both nerve preservation and nerve dissection group was assessed and in both groups no change noticed because both groups have no pain.
Mild chronic groin pain during coughing at six months follow up in both nerve preservation and nerve dissection group was assessed and in both groups no change noticed because both groups have no pain.
Moderate chronic groin pain during coughing at three months follow up in both nerve preservation and nerve dissection group was assessed and in both groups no change noticed because both groups have no pain.
Moderate chronic groin pain during coughing at six months follow up in both nerve preservation and nerve dissection group was assessed and in both groups no change noticed because both groups have no pain.
Severe chronic groin pain during coughing at three months follow up in both nerve preservation and nerve dissection group was assessed and in both groups no change noticed because both groups have no pain.
Severe chronic groin pain during coughing at six months follow up in both nerve preservation and nerve dissection group was assessed and in both groups no change noticed because both groups have no pain.
Mild chronic groin pain during climbing stairs at three months follow up in both nerve preservation and nerve dissection group was assessed. One patient in nerve preservation group had pain that is 3% of the total group population and the P- Value was 0.313 which is statistically not significant (Table 4)(Figure 1).
| Groups | MILDPAIN3MCLIMBING | Total | |
| No | Yes | ||
| Nerve division | 30 | 0 | 30 |
| Nerve preservation | 29 | 1 | 30 | Total | 59 | 1 | 60 |
Mild chronic groin pain during climbing stairs at six months follow up in both nerve preservation and nerve dissection group was assessed. One patient in nerve preservation group had pain that is 3% of the total group population and P-Value was 0.313 which is statistically not significant (Table 5)(Figure 2).
| Groups | MILDPAIN3MCLIMBING | Total | |
| No | Yes | ||
| Nerve division | 30 | 0 | 30 |
| Nerve preservation | 29 | 1 | 30 | Total | 59 | 1 | 60 |
Moderate chronic groin pain during climbing stairs at three months follow up in both nerve preservation and nerve dissection group was assessed and in both groups no change noticed because both groups have no pain.
Moderate chronic groin pain during climbing stairs at six months follow up in both nerve preservation and nerve dissection group was assessed and in both groups no change noticed because both groups have no pain.
Severe chronic groin pain during climbing stairs at three months follow up in both nerve preservation and nerve dissection group was assessed and in both groups no change noticed because both groups have no pain.
Severe chronic groin pain during climbing stairs at six months follow up in both nerve preservation and nerve dissection group was assessed and in both groups no change noticed because both groups have no pain.
Mild chronic groin pain during brisk walking at three month follow up in both nerve preservation and nerve dissection group was assessed. Three patients from nerve dissection group had pain that is 10% of the total group population and fifteen patients from nerve preservation group had pain that is 50% of the group population and P-Value was 0.001 which is statistically significant (Table 6)(Figure 3).
| Groups | MILDPAIN3MCLIMBING | Total | |
| No | Yes | ||
| Nerve division | 27 | 3 | 30 |
| Nerve preservation | 15 | 15 | 30 | Total | 42 | 18 | 60 |
Mild chronic groin pain during brisk walking at six months follow up in both nerve preservation and nerve dissection group was assessed. Seven patients from nerve dissection group had pain that is 23% of the total group population and twelve patients from nerve preservation group had pain that is 60% of the total group population and P-Value was 0.004 which is statistically significant (Table 7)(Figure 4).
| Groups | MILDPAIN3MCLIMBING | Total | |
| No | Yes | ||
| Nerve division | 23 | 7 | 30 |
| Nerve preservation | 12 | 18 | 30 | Total | 35 | 25 | 60 |
Moderate chronic groin pain during brisk walking at three month follow up in both nerve preservation and nerve dissection group was assessed. None of the patient from nerve dissection group had pain but four patients from nerve preservation group had pain that is 13.3% of the total group population and P-Value was 0.038 which is statistically in significant (Table 8)(Figure 5).
| Groups | MILDPAIN3MCLIMBING | Total | |
| No | Yes | ||
| Nerve division | 30 | 0 | 30 |
| Nerve preservation | 26 | 4 | 30 | Total | 56 | 4 | 60 |
Moderate chronic groin pain during brisk walking at six months follow up in both nerve preservation and nerve dissection group was assessed. None of the patient from nerve dissection group had pain but two patients from nerve preservation group had pain that is 6.6% of the total group population and P-Value was 0.150 which is statistically in significant (Table 9)(Figure 6).
| Groups | MILDPAIN3MCLIMBING | Total | |
| No | Yes | ||
| Nerve division | 30 | 0 | 30 |
| Nerve preservation | 28 | 2 | 30 | Total | 58 | 2 | 60 |
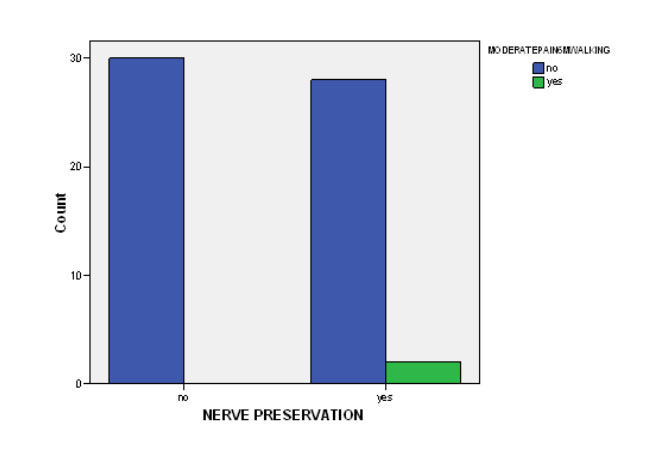 Figure 6: Presentation of patients experience moderate pain after brisk
walking / jogging at six months follow up.
Figure 6: Presentation of patients experience moderate pain after brisk
walking / jogging at six months follow up.Severe chronic groin pain during brisk walking at three months follow up in both nerve preservation and nerve dissection group was assessed. None of the patient from any group had pain.
Severe chronic groin pain during brisk walking at six months follow up in both nerve preservation and nerve dissection group was assessed. None of the patient from any group had pain.
Mild groin numbness at three months follow up was assessed in both groups. Six patients from nerve dissection group that is 20 % of the total group population and nine patients from nerve preservation group that is 30% of the total group population had numbness. P-Value was 0.371 which is statistically in significant (Table 10)(Figure 7).
| Groups | MILDPAIN3MCLIMBING | Total | |
| No | Yes | ||
| Nerve division | 24 | 6 | 30 |
| Nerve preservation | 21 | 9 | 30 | Total | 45 | 15 | 60 |
Mild groin numbness at six months follow up was assessed in both groups. Ten patients from nerve dissection group that is 33.3% of total group population and nine patients from nerve preservation group that is 30% of the total group population had numbness. P-Value was 0.781 which is statistically in significant (Table 12)(Figure 8).
| Groups | MILDPAIN3MCLIMBING | Total | |
| No | Yes | ||
| Nerve division | 20 | 10 | 30 |
| Nerve preservation | 21 | 9 | 30 | Total | 41 | 19 | 60 |
Moderate groin numbness at three months follow up was assessed in both groups. None of the patients of either group had numbness.
Moderate groin numbness at six months follow up assessed in both groups. None of the patients of either group had numbness.
Severe groin numbness at three months follow up was assessed in both groups. None of the patients of either group had numbness.
Severe groin numbness at six months follow up was assessed in both groups. None of the patients of either group had numbness.
Chronic post operative groin pain after inguinal hernia mesh repair is becoming one of the significant problem [4]. It is important to differentiate between the chronic and acute post operative pain. Early post operative is usually seen soon after surgical intervention and easily managed with analgesics and generally resolves with in 15-30 days of surgery without the need of any further treatment [4]. On the other hand moderate to severe groin pain generally seen after surgical procedure and persisting beyond the normal tissue healing time assumed to be three months is considered to be the chronic post operative pain [4,5]. Several factors have been proposed as predictors of chronic pain such as experience of the surgeon, surgery due to recurrence, damage to the inguinal nerve, partial division, neuroma formation, nerve entrapment during mesh implantation [4]. The nerve usually divided or ligated when its course in the operating field would lead to the risk of injury or if it interfere with the positioning of mesh. Leaving the injured nerve intact will continue to generate the pain signals and remain exposed to the neuroma formation. It is important to resect the nerve as proximal as possible, so that it would not interfere or come in to contact with the mesh. One of the proposed mechanisms for the development of post operative chronic pain is the implantation and fibrosis induced by mesh which is in close proximity to the nerve. Routine ilioinguinal nerve excision has been considered as one of the means to avoid these complications.
The earlier study to investigate the effects of this procedure was carried out by Ravichandran and his colleague [4]. They conducted a pilot study comparing preservation or division of the ilioinguinal nerve in the inguinal hernia open mesh repairs. Twenty patients with bilateral inguinal hernia were randomized to nerve preservation on one side and division on other. At six months post operatively, pain was present in one of 20 patients (5%) on the nerve preserved side versus zero of 20 patients (0%) on the nerve division side. Numbness was present in zero of 20 patients (0%) on the nerve preserved side versus two of 20 patients (10%) on the nerve divided side. These differences were all non significant and led the author to conclude that elective division of ilioinguinal nerve was not associated with a significant decrease in post operative pain in inguinal hernia mesh repairs. However subsequent studies with larger sample size have shown statistically significant decrease in the incidence of post operative pain in the nerve excision group versus nerve preservation group.
Malekpour et al, Dittrick et al, Mui et al. etc showed that the incidence of post operative chronic groin pain was significantly lower in neurectomy group as compare to the nerve preservation group. On the other hand a study done by Picchio M et al has been failed to show any relationship between nerve preservation and division with chronic post operative groin pain.
In a net shell we have both types of studies in literature favoring ilioinguinal nerve division/preservation to be beneficial for reduction of chronic post operative groin pain after elective inguinal hernia mesh repair.
This study has been conducted to assess the effect of ilioinguinal neurectomy on chronic post operative pain and groin numbness after inguinal hernia mesh repair. In this study total 60 patients were selected who fall in the inclusion criteria of the study and were randomly divided in to two groups that is nerve preservation (group A) and nerve division (group B). Mean age of population in group A is 42.96 +/- 17.76 an in group B is 54.23 +/- 15.0. All patients were male as female gender was exclusion criteria.
Both groups were compared in term of post operative chronic pain and groin numbness. Patients were followed on OPD basis at three and six months. All patients were challenged by being asked to complete a series of tasks before pain assessment, including rest, after coughing, after climbing stairs and after brisk walking/jogging for five minutes. Therefore we were able to examine the effects of exertion on groin pain after surgery; this will better express their experience of pain during routine daily activities. Pain score was assessed using visual analog score as mild, moderate and severe. Groin numbness was assessed at rest using same visual analog score after comparing with the opposite non surgical site. Our randomized study revealed that the incidence of chronic groin at rest and while coughing was similar between the two groups which is similar to the findingsof Picchio et al. however chronic pain on vigorous walking/ jogging was higher in nerve preservation group as compare to the neurectomy group where the P-value was statistically significant (P-Value at three month follow up was 0.001 and at six months follow up it was 0.004). This also reflect that the effects of ilioinguinal neurectomy during hernia repair has better post operative results regarding daily activities and quality of life. On the other hand groin numbness between the two groups has similar out come and the P value is statistically insignificant [6-8].
The results of these prospective randomized control trials demonstrate that prophylactic ilioinguinal neurectomy during Lichtenstein tension free inguinal hernia repair decreases the incidence of exertional chronic post operative pain as compare to the nerve preservation group. However the cutaneous neurosensory disturbance/groin numbness between the two groups has no difference in term of outcome. So it has been recommended that ilioinguinal neurectomy should be a routine step during inguinal hernia mesh repair as it will improve patients over all quality of life and has no effects on neurosensory disturbance.
