 Journal of Clinical and Biomedical Investigation
PROVIDES A UNIQUE PLATFORM COVERING SCIENTIFIC KNOWLEDGE IN BIOMEDICAL SCIENCES AND CLINICAL RESEARCH
Journal of Clinical and Biomedical Investigation
PROVIDES A UNIQUE PLATFORM COVERING SCIENTIFIC KNOWLEDGE IN BIOMEDICAL SCIENCES AND CLINICAL RESEARCH
 Journal of Clinical and Biomedical Investigation
PROVIDES A UNIQUE PLATFORM COVERING SCIENTIFIC KNOWLEDGE IN BIOMEDICAL SCIENCES AND CLINICAL RESEARCH
Journal of Clinical and Biomedical Investigation
PROVIDES A UNIQUE PLATFORM COVERING SCIENTIFIC KNOWLEDGE IN BIOMEDICAL SCIENCES AND CLINICAL RESEARCH
Vitrag Shah*
Physician and Chief Intensivist, Velocity Hospital, Surat, Gujarat, India
Correspondence to: Vitrag Shah, Physician and Chief Intensivist, Velocity Hospital, Surat, Gujarat, India.
Received date: November 24, 2022; Accepted date: December 21, 2022; Published date: December 28, 2022
Citation: Shah V (2022) Aerosol Generating Procedures-How to Manage? J Clin Biomed Invest. 2(2): pp. 37. doi:
10.52916/jcbi224018
Copyright: ©2022 Shah V. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits
unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Aerosol Generating Procedures (AGP) leads to high risk of exposure to healthcare workers and leading to acute respiratory infections. After COVID-19 pandemic, management of AGPs have been reinforced and many innovations have occurred to minimize risk of airborne transmission during AGPs. In this article we will be discussing difference between aerosol and droplet, various AGPs, factors affecting transmission, various methods to minimize risk in AGPs etc.
Aerosol, Droplet, NIV, Nebulization, Isolation, Infection control
Aerosols are tiny respiratory particles that are small and light enough to stay suspended in the air for long periods of time, travel beyond 6 feet from the source patient, and able to penetrate surgical masks [1]. Even when an infectious person is more than 6 feet away, aerosols have the ability to travel and infect others. Usual size of aerosol is <10 micrometers. Droplets are larger and heavier respiratory particles which can travel up to 6 feet, but then they fall to the ground. Aerosol can stay in air upto half an hour and in indoor areas if room is not ventilated, it can stay even longer. When disease is transmitted by aerosol, it is called aerosol transmission and transmitted by droplets, it is called droplet transmission. COVID-19 is transmitted by droplets but in poorly ventilated indoor area and during aerosol generating procedures, it can be transmitted by aerosol too.
Aerosol generating procedures is any medical/healthcare procedure which creates increased risk of transmission of aerosol borne contagious disease by generating aerosol (Table 1).
Table 1: Aerosol generating procedures.
|
Nebulization |
Broncoscopy |
|
Non-Invasive Ventilation (NIV)/Bag and mask ventilation |
Cardio-Pulmonary Resuscitation (CPR) |
|
High flow oxygen |
Coughing/Sneezing/Sputum induction |
|
High Flow Nasal Cannula (HFNC) |
Spirometry |
|
Intubation |
Tracheostomy |
|
Suctioning |
Chest physiotherapy |
Forced air from respiratory mucosa: NIV, Spirometry, coughing, loud speaking etc.
Severity of disease and symptoms: Symptomatic patients shed more virus as they tend to cough, sneeze more and become breathless on exertion.
Distance and ventilation: Higher risk of catching virus within 6 feet of contact with source patient and higher risk in indoor poorly ventilated space.
Duration: Longer time one is exposed to source patient/aerosol, higher risk of catching infection. This is explained by fact that once one member of household is infected, higher chances other members are also infected even in mild symptomatic contact. Combining all four risk factors increase probability of catching infection further, e.g. severely symptomatic patients in poorly ventilated area for longer period of time with excessive coughing and breathing difficulty (e.g. in Intensive Care Unit (ICU)/High Dependency Unit (HDU) without negative pressure isolation).
Routine precautions: Routine infection control measures like proper Personal Protective Equipment (PPE) and mask/ respirator usage, hand hygiene, isolation practices, disinfection of equipment, environmental cleaning, and spacing of beds etc must be followed. PPE kit and hand hygine are most important for minimizing risk of transmission to healthcare workers when working in high risk areas and caring suspected COVID-19 patients. N-95 mask with proper fit must be worn while performing any aerosol generating procedures. There are some in vitro studies of povidone-iodine nasal solution to mitigate virus transmission. It has been found to be effective for contact time as short as 15 seconds and even in 0.5% concentration, but further clinical studies are needed to establish benefit. Now a days even 0.5% betadine oral and throay spray is also available which can be used prior to any aerosol generating procedures. Following extra precautions should be taken while handling COVID-19 patients with aerosol generating procedures [2].
Maximize air exchanges and negative pressure isolation: (a) Use area with maximum number of air changes per hour to manage critically ill COVID-19 patient to minimize the risk of cross-infections. Either natural ventilation with airflow of at least 160 L/s per patient or negative pressure rooms with at least 12 air changes per hour is recommended during any aerosol generating procedures. HEPA filter unit is required for the recirculation of air. (b) Minimize transport of patient and minimize opening and closing of doors [2-4].
Oxygen/High Flow Nasal Cannula (HFNC) oxygen therapy: (a)Use minimum flow of oxygen required. (b) Use surgical/N95 mask over patient’s face whenever using nasal cannula, HFNC or any patient without artificial airway to minimize aerosol spread.
Non-Invasive Ventilation (NIV): (a) Prefer HFNC over NIV. (b) Use full facemask over nasal or oronasal mask. Use non-vented mask, avoid vented mask. (c) Use ICU ventilator with dual limb circuit over portable BIPAP machine with single limb circuit as vented mask required for single limb circuit which increases the risk of aerosol spread over non vented mask used in dual limb circuit. (d) If using NIV, use minimum pressure (Pi/PS). (e) Ensure tight mask seal to minimize leak and aerosol spread due to leak. (f) Use viral filter at expiratory end of circuit and between catheter mount and Y-Piece of ventilator circuit. (g) Helmet NIV can be used as it is sealed and closed space in helmet which minimize aerosol spread. However disadvantages with Helmet NIV is increase in dead space, claustrophobia, difficulty in suction and feeding etc, so it is not much popular [5,6] (Figure 1).
 Figure 1: (A) HME filter between catheter mount and Y-piece (Left), (B) HME
(without filter) at expiratory limb of ventilator circuit (right).
Figure 1: (A) HME filter between catheter mount and Y-piece (Left), (B) HME
(without filter) at expiratory limb of ventilator circuit (right).Intubation and extubation: (a) Keep low threshold for intubation to avoid crash intubation and minimize risk of aerosol spread with NIV. (b) Endotracheal intubation should be done by most experienced provider to minimize number of attempts and risk of transmission. (c) Rapid sequence intubation should be done. Intubation should be done after giving proper sedatives and relaxants only to minimize aerosol generation. (d) Use video laryngoscope if available to avoid in close contact with airway. (e) Use HME filter when doing bag and mask ventilation or mask ventilation with ventilator. (f) Clamp ET tube or attach viral filter to ET tube while intubation. (g) Inflate cuff immediately after intubation to keep cuff pressure 25-30 and ensure there is no leak. (h) Aerosol box use during intubation is controversial but it can be used during extubation to minimize aerosol spread. (i) Use mild sedation or intracuff lidocaine to avoid coughing during extubation.
Mechanical ventilation, broncoscopy and suctioning: (a) Do O2 suction (100% FiO2 for 1 minute) and keep ventilator on standby whenever disconnecting patient from ventilator. (b) Use disposable expiratory valve and new flow sensor if possible. (c) Use disposable accessories like BP cuff, SPO2 probe, Electrocardiogram (ECG) leads etc if available. (d) Cover monitor, ventilator and other equipment with transparent sheet/plastic drape. (e) Use minimum pressure/tidal volume required to minimize peak pressure and avoid leak. (f) Use close suction if available and avoid routine suctioning. (g) Avoid broncoscopy unless absolutely necessary (Figure 2).
Nebulization: (a). Do not use nebulization routinely. (b) Use Metered Dose Inhaler (MDI) with spacer/MDI alone over nebulizer whenever required (Figure 3). (c) Use special kind of circuits/T-Connector with auto shutoff function to avoid circuit disconnection during nebulization (Figure 4). (d) Use special kind of HME filter with on-off switch to avoid circuit disconnection during nebulization (Figure 5).
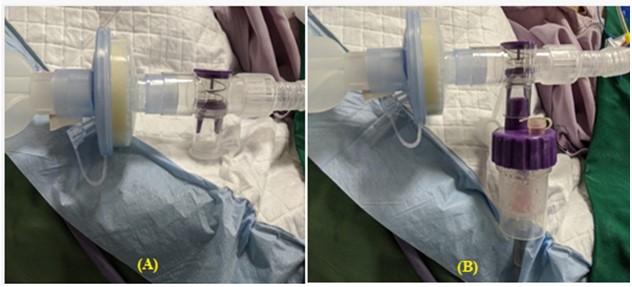 Figure 4: Novel T-connector for nebulization with auto shut-off function. (A) Without nebulizer chamber (left); and (B) nebulizer chamber attached to T-connector (right).
Figure 4: Novel T-connector for nebulization with auto shut-off function. (A) Without nebulizer chamber (left); and (B) nebulizer chamber attached to T-connector (right). Figure 5: (A) HME filter between catheter mount and Y-piece (Left), (B) HME
(without filter) at expiratory limb of ventilator circuit (right).
Figure 5: (A) HME filter between catheter mount and Y-piece (Left), (B) HME
(without filter) at expiratory limb of ventilator circuit (right).In summary, many routine procedures in hospital and clinic are AGPs which are underlooked and simple preventive measures will minimize risk of exposure to healthcare workers. Apart from PPE and isolation, many more measures we can do like using novel HME filters, close suction, T-Connectors with auto shutoff function for nebulization etc. This article is to highlight importance of other preventive measures apart from PPT kit and isolation and sensitive paramedical staff to implement same in routine practice.
