 Journal of Obstetrics and Gynecological Surgery
A PLATFORM FOR SCIENTIFIC INQUIRY IN THE FIELD OF OBSTETRIC AND GYNECOLOGY FIELD
Journal of Obstetrics and Gynecological Surgery
A PLATFORM FOR SCIENTIFIC INQUIRY IN THE FIELD OF OBSTETRIC AND GYNECOLOGY FIELD
 Journal of Obstetrics and Gynecological Surgery
A PLATFORM FOR SCIENTIFIC INQUIRY IN THE FIELD OF OBSTETRIC AND GYNECOLOGY FIELD
Journal of Obstetrics and Gynecological Surgery
A PLATFORM FOR SCIENTIFIC INQUIRY IN THE FIELD OF OBSTETRIC AND GYNECOLOGY FIELD
Kulvinder Kochar Kaur1* , Gautam Allahbadia2, Mandeep Singh3
, Gautam Allahbadia2, Mandeep Singh3
1Scientific Director, Dr Kulvinder Kaur Centre for Human Reproduction, G.T.B. Nagar, Jalandhar-144001, Punjab, India
2Scientific Director, Ex-Rotunda-A Centre for Human Reproduction, Kalpak Garden, Bandra(W)-400040, Mumbai India
3Consultant Neurologist, Swami Satyanand Hospital, Near Nawi Kachehri, Baradri, Ladowali Road, Jalandhar, Punjab, India
Correspondence to: Kulvinder Kochar Kaur, Scientific Director, Dr Kulvinder Kaur Centre for Human Reproduction, G.T.B. Nagar, Jalandhar-144001, Punjab, India
Received date: February 17, 2022; Accepted date: March 15, 2022; Published date: March 22, 2022
Citation: Kaur KK, Allahbadia G, Singh M (2022) Dependability of the Sperm Chromatin Dispersion (SCD) Assay for Recurrent Sperm DNA Damage Evaluation of
Sperm DNA Fragmentation (SDF) in Men with Presentation of Infertility-A Short Communication. J Obst Gynecol Surg 3(1): pp. 1-3. doi: 10.52916/jogs224021
Copyright: ©2022 Kaur KK, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted
use, distribution and reproduction in any medium, provided the original author and source are credited
How the male attributes in the generation of a healthy embryo, there exists a need for a sperm that is of good quality with minimum genome injury whose estimationis usually are done by the determination of sperm Deoxyribonucleic Acid (DNA) breakdown or the Sperm DNA Fragmentation (SDF). SDF usually guides with regards to the quality of sperm chromatin in case of men with a presentation of infertility. The causes attributed are the capacity of side actions of escalation of SDF amounts on natural fertility, embryo generation along with implantation, risk of miscarriage along with health of the newborn [1]. Earlier we detailed the role of SDF in Intracytoplasmic Sperm Injection (ICSI) with use of Time Lapse Microscopy (TLM) simultaneously [2]. SDF represents a marker of chromatin injury, takes place at the time of spermiogenesis, halt in the epididymis along withpost ejaculation inview of various factors that are not unique like varicocoele, insufficient life style like toxic exposure secondary to occupational along with experimental factors, aging as well as infections [3]. For the birth of a healthy newborn, genomically healthy sperms are necessary, while enhancement of sperms with injured chromatin in the human ejaculate might result in non stabilization of the genome at the time of fertilization as well as embryogenesis [4]. Thus it has been pointed that the evaluation of sperm chromatin at a molecularlevel might aid in its provision of the paternal factor for infertility, besides point to decide what treatment actions might be feasi ble for enhanced sperm chromatin quality [5].
A key action of the semen evaluation with regards to clinical andrology laboratory is if estimation of a variable by a single investigator in the same person at 2 separte time periods gives the akin results. Considerable intrindividual differences with regards to routine semen factors has been well revealed [6]. These differences get reasoned out by environmental, technical along with biological factors [7]. Conversely, studies that evaluated the intrapersonal differences of SDF over time duration are rare [8], with no study documenting the utilization of Sperm Chromatin Dispersion (SCD) assay. This SCD is dependent on the basis that sperm along with sperm DNA fragmentation are incapable of generation of a typical halo of thedispersed DNA loops that is classically seen in nonfragmented DNA [9]. In case of SCD sperm suspension are embedded within agarose gel on slide along with treated with a solution that is acid denatured for the production of a limited single strand DNA motifs at the region of the, existent single or double strand breaks. The denaturation is halted, along with spermatozoa getting exposure to a solution that is lysing for deletion of the sperm membrane along with nuclear proteins. Finally, the slides get stained, along with the proportion of sperms with nondispersed along with dispersed chromatin loops get manually evaluated under fluorescence or bright field microscopy [1,10]. The typical halos are a kin to the open loops that are attached to the nuclear structure as visualized in sperm with low or no SDF. Conversely sperms revealing SDF display minimum or no halos.
Enough intactness of DNA is key for achieving successful fertilization, generation of embryo, implantation, along with pregnancy development, in view of a minimum of 50% of the embryonic genome being accorded [10]. Thus the sperm DNA intactness is hence believed to be a significant marker of the fertility capacity of the spermatozoa. Multiple intrinsic in addition to extrinsic risk factors for SDF are existent that are inclusive of abnormalities in the chromatin condensation, apoptosis that is abortive, as well as Oxidative Stress (OS) [10]. Hence having a SDF testing that is trustworthy is necessary for the assessment with regards to the treatmentof a couple whose presentation is infertility.
More recently, Esteves et al. [11], described a prospective study where assessment of how much trust could be laid on the sperm chromatin dispersion test for the assessment of sperm fragmentation. Their publication was inclusive of a concentrated patients population, the sample size that was enough, the experimental protocol that was well described in full details, negative along with positive controls besides statistical detailing along with utilization of the particular statistical tools in details. The aim of Esteves et al. [11], was the assessment of intra individual consensus of the sperm chromatin dispersion test outcomes for evaluation of SDF in men presenting with infertility.
They did a classification of DNA fragmentation into 3 namely
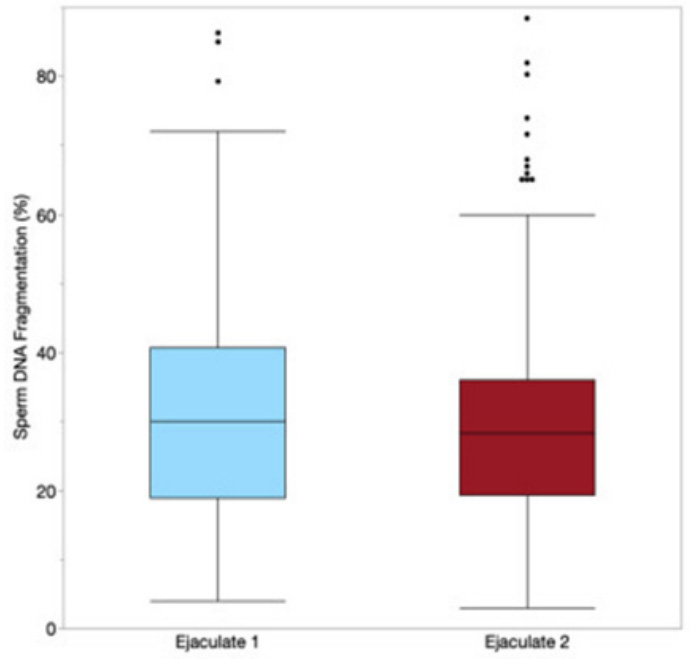
They illustrated that lower differences in recurrent investigations, in normal or high DNA fragmentation, since >80% of recurrent samples as per these classifications continued to remain in the same subgroup or category. The ones where alterations actually occurred, did so in the intermediate class. Conversely, 33% of men with infertility presentation with the prior intermediate DNA fragmentation altered to the normal of high subgroups of SDF on recurrent investigation (Figure 1 and 2).
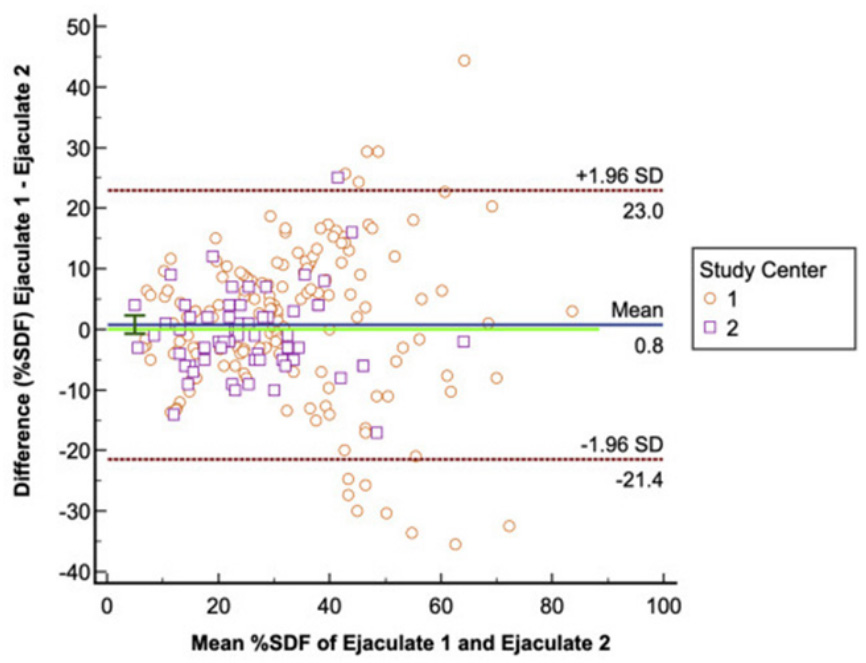
Hence this publication illustrated as per the statistical language a clinical observation that possesses the capacity of being significant with regards to existence of cases where the SDF value impacts the decision made by the treating medical physician. Like there is an existence of a documented part for testicular sperm extraction in a setti ng where earlier In Vitro Fertilization(IVF) had failed with the male possessing high SDF in his ejaculated sperm.
The existent work of Esteves et al. [11], gives us an opportunity of contrasting the SDF observations in the same person subsequent to various treatment protocols, like in testicular sperm extraction, varicocoele surgery along with utilization of anti oxidants, with their confidence sustenance that variation with time duration would not bother the data. In a systematic review that got carried out by Zini as well as Dohle [12], tried quantitation of association amongst varicocoele correlated SDF along with SDF control. Assessment of 7 studies was performed as well as their observation was that of 6/7 studies (n=279 patients), patients that possessed a varicocoele illustrated significant higher SDF in contrast to fertile controls.
Moreover, Wang et al. [13], in a follow up publication documented a meta-analysis of 6 studies (n=177 patients), whose presentation was the action of varicocoele correction on alterations of the concentrations of the DNA injury. As per these workers varicocoele correction significantly resulted in enhancement of DNA intactness. Such outcomes can be depended upon with greater reliance with the knowledge that repeated SDF prior as well as subsequent, to any kind of treatment does not impact by recurrent investigation.
Usually men are seen following a failed IVF with female assessment having been normal along with a normal semen assessment as per the World Health Organization (WHO) criteria. Additionally, functional sperm tests like SDF can give extra knowledge along with isolation of patients for aiding in finding the etiology of infertility. With this information that there is existence of low intraperso nal difference with SDF now gives provision of trustfulness in the clinical significance along with the anticipationvalue of this laboratory investigation [14].
With this information that there is existence of low intrapersonal difference with SDF now gives provision of trustfulness in the clinical significance along with the anticipationvalue of this laboratory investigation (SCD) [12,14]. Hence the SCD is a dependable test with intrapersonal difference of thepersons that conducted the tests usually are similar other than occasional difference.
