 Journal of Obstetrics and Gynecological Surgery
A PLATFORM FOR SCIENTIFIC INQUIRY IN THE FIELD OF OBSTETRIC AND GYNECOLOGY FIELD
Journal of Obstetrics and Gynecological Surgery
A PLATFORM FOR SCIENTIFIC INQUIRY IN THE FIELD OF OBSTETRIC AND GYNECOLOGY FIELD
 Journal of Obstetrics and Gynecological Surgery
A PLATFORM FOR SCIENTIFIC INQUIRY IN THE FIELD OF OBSTETRIC AND GYNECOLOGY FIELD
Journal of Obstetrics and Gynecological Surgery
A PLATFORM FOR SCIENTIFIC INQUIRY IN THE FIELD OF OBSTETRIC AND GYNECOLOGY FIELD
Anubha Bajaj*
Consultant Histopathologist, AB Diagnostics, India.
Correspondence to: Anubha Bajaj, Consultant Histopathologist, AB Diagnostics, India.
Received date: May 15, 2023; Accepted date: June 08, 2023; Published date: June 15, 2023
Citation: Bajaj A. Coelenterate and Germinal-Müllerian Papilloma Cervix: A Mini-Review. J Obst Gynecol Surg. 2023;3(2): 7-9. doi:10.52916/jogs234033
Copyright: ©2023 Bajaj A. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use,
distribution and reproduction in any medium, provided the original author and source are credited.
Müllerian papilloma of uterine cervix is an infrequently encountered, benign neoplasm simulating the malignant botyroid rhabdomyosarcoma. Of obscure aetiology or pathogenesis, Müllerian papilloma is posited to emerge from anomalous embryological tissue remnants amalgamated during foetal growth and diverse stages of foetal development. Generally asymptomatic, Müllerian papilloma may delineate abnormal vaginal bleeding, spotting and/or vaginal discharge, abdominal pain, pelvic pain, lumbar pain, discomfort, difficulty in micturition or primary infertility in adulthood due to mechanical obstruction of cervix. Neoplasm is comprised of papillary stalks layered by mucinous epithelium with focal squamous metaplasia and an extensively cellular and fibrous encompassing stroma. Tumefaction appears immune reactive to CK7, CA125 or Epithelial Membrane Antigen (EMA). Müllerian papilloma of uterine cervix requires segregation from neoplasms such as botyroid rhabdomyosarcoma, cervical clear cell carcinoma or cervical polyp demonstrating superficial ulceration, haemorrhage or secondary infections. Müllerian papilloma of uterine cervix may be appropriately discerned with competent history and physical examination with pelvic evaluation, abdominal ultrasonography, Computerized Tomography (CT), contrast enhanced computerized tomography or Magnetic Resonance Imaging (MRI) of abdomen and pelvis. Müllerian papilloma of uterine cervix may be appropriately managed with comprehensive, localized surgical extermination of the neoplasm.
Müllerian papilloma, Embryological tissue remnants, Botyroid rhabdomyosarcoma, Computerized Tomography (CT), Magnetic Resonance Imaging (MRI)
Müllerian papilloma of uterine cervix is an exceptionally discerned, benign neoplasm simulating the malignant botyroid rhabdomyosarcoma. Müllerian papilloma of uterine cervix is additionally designated as cervical Müllerian papilloma, intramural papilloma of uterine cervix or mesonephric papilloma of uterine cervix.
The infrequent, benign Müllerian papilloma of uterine cervix preponderantly incriminates infants or young females. Asymptomatic instances may be subjected to meticulous observation. Therapeutic intervention with cogent surgical management of the neoplasm is accompanied by excellent prognostic outcomes.
The infrequent Müllerian papilloma of uterine cervix is preponderantly observed in girls between 2 years to 5 years although young girls between one year to 9 years may be incriminated. Generally, the benign, polypoid lesion of cervix or vagina may be discerned within young girls or adult women. Tumefaction arising in childhood may be confined to the vagina.
A specific ethnic or racial predilection or cogent contributory factors are absent. Of obscure aetiology or pathogenesis, Müllerian papilloma of uterine cervix is posited to emerge from anomalous embryological tissue remnants amalgamated during foetal growth and various stages of foetal development. Of Müllerian origin, neoplasm appears confined within superficial segments of uterine cervix or vagina [1,2].
Müllerian papilloma configures a polyp-like lesion confined to the uterine cervix. Generally asymptomatic, tumefaction may induce abnormal vaginal bleeding or vaginal discharge.
Neoplasm may represent as a polyp or an intramural lesion confined to uterine cervix or vagina. Neoplasm represents with vaginal bleeding within female infants (1,2). Majority of neoplasms are asymptomatic. Nevertheless, Müllerian papilloma of uterine cervix may be accompanied by
The benign Müllerian papilloma of uterine cervix may be misinterpreted as cervical cancer, cervical polyp demonstrating superficial ulceration, haemorrhage or secondary infections and primary infertility in adulthood due to mechanical obstruction of cervix. Besides, the predominantly polypoid tumefaction may undergo mechanical injury with occurrence of torsion or twisting along with excruciating abdominal pain [2,3].
Grossly, polyp-like lesions are <2 centimetre in diameter. Tumefaction may be multifocal and is preponderantly confined to uterine cervix or vagina. Upon microscopy, neoplasm is comprised of papillary stalks layered by mucinous epithelium. Focal squamous metaplasia may be encountered. Circumscribing stroma is extensively cellular and fibrous [3,4].
Neoplasm represents with papillary, glandular or cystic architecture. Papillary or glandular structures are layered with cuboidal or low columnar epithelium. Neoplastic papillae are encompassed by myxoid stroma incorporated with an inflammatory cell infiltrate and vascular articulations [3,4]. Cellular or nuclear atypia is absent. Mitotic activity is minimal [3,4].
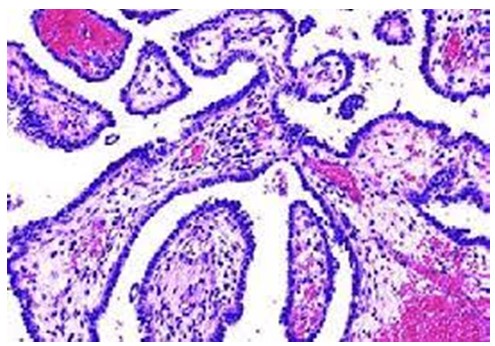 Figure 1: Mullerian papilloma depicting papillary and glandular structures layered by cuboidal to low columnar epithelium circumscribed by a cellular, fibrotic stroma infiltrated by chronic inflammatory cells and vascular articulations.
Figure 1: Mullerian papilloma depicting papillary and glandular structures layered by cuboidal to low columnar epithelium circumscribed by a cellular, fibrotic stroma infiltrated by chronic inflammatory cells and vascular articulations. 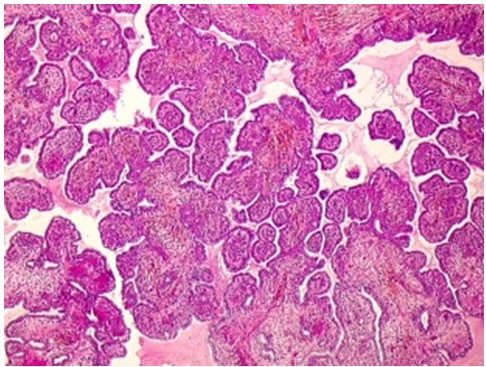 Figure 2: Müllerian papilloma delineating papillary and glandular articulations lined by cuboidal to low columnar epithelium surrounded by a cellular, fibrotic stroma infiltrated by chronic inflammatory cells and vascular articulations.
Figure 2: Müllerian papilloma delineating papillary and glandular articulations lined by cuboidal to low columnar epithelium surrounded by a cellular, fibrotic stroma infiltrated by chronic inflammatory cells and vascular articulations. Embryonic Müllerian duct anomaly is classified as: Class I: comprised of uterine agenesis or uterine hypoplasia. Further segregated as:
Class II: comprised of unicornuate uterus or unicornis unicollis and represents up to 25% lesions. Further segregated as:
Class III: Comprised of uterus didelphys and represents up to 11% lesions.
Class IV: Comprised of bicornuate uterus and represents up to 39% lesions. Further segregated as
Class V: comprised of septate uterus and appears as a commonly discerned anomaly in up to 55% lesions. Further segregated as
Class VI: Comprised of arcuate uterus and represents ~7% lesions.
Class VII: Comprised of in utero Diethylstilbestrol (DES) exposure with the occurrence of T-shaped uterus [3,4].
Müllerian papilloma of uterine cervix appears immune reactive to CK7, CA125 and Epithelial Membrane Antigen (EMA). Tumour cells appear immune non reactive to CK20, Carcinoembryonic Antigen (CEA) or Smooth Muscle Actin (SMA) [5,6]. Müllerian papilloma of uterine cervix requires segregation from neoplasms such as botyroid rhabdomyosarcoma.
Morphologically, cervical Müllerian papilloma requires segregation from cervical clear cell carcinoma [5,6]. Müllerian papilloma of uterine cervix may be appropriately discerned with
Benign Müllerian papilloma of uterine cervix may be appropriately managed with comprehensive, localized surgical extermination of the neoplasm. Tumour reoccurrence may ensue [5,6].
Precise and applicable therapeutic strategies are comprised of
Surgical intervention may be associated with injury to circumscribing skeletal muscles, peripheral nerves or vascular articulations. Post-surgical infection upon wound site may ensue. Incomplete surgical eradication of the neoplasm may be associated with tumour reoccurrence. Prognostic outcomes are excellent [5,6]. Circumvention of emergence of Müllerian papilloma of uterine cervix remains undefined. However, cogent regular screening with physical examination and relevant scans is recommended [5,6].
The authors declare no conflict of interest.
No.
